
Pre-emptive first deceased donor renal transplant: A matched cohort study
Antonio Franco Esteve1, Elena de la Cruz1, Francisco Javier Perez Contreras1, Patricio Más-Serrano2.
1Department of nephrology, Hospital Dr Balmis Alicante, Alicante, Spain; 2Farmacy, Hospital Dr Balmis Alicante, Alicante, Spain
Renal transplant is the treatment of choice in patients with chronic renal insuficiency which require replacement therapy. Dialysis is usually a previous step but not mandatory before transplant and pre-emptive transplant from living or deceased donors is possible.
Since 2007 we started a program of pre-emptive renal transplant from deceased donors and the objetive of this study is to evaluate the results.
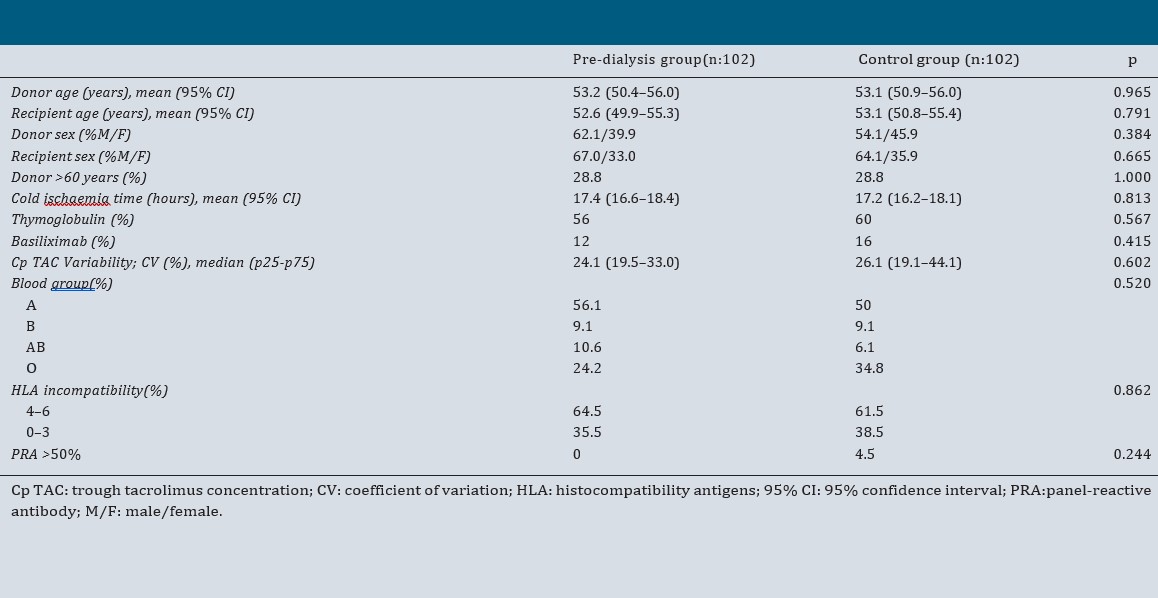
This is a retrospective observational study with matched cohorts. Recipients who received first grafts from deceased donors in our hospital between 2007-2016 were enroled. Two cohorts of 102 recipients were compared: a predialysis group who received a pre-emptive transplant from deceased donors and a control group of patients who were transplanted on dialysis. Inclusion criteria of pre-emptive recipients were glomerular filtration rate under 15 ml/mn(CKDP), a estimated time to start dialysis less than 6 months and more than 1 year of follow-up. Both groups were matched by age and gender of donor and recipient, donors over 60 years, cold isquemia, blood group and transplant date between pre-emptive and control recipient which must be less than 7 days. The immunological status was evaluated via donor/ recipient compatibility and the performed antibodies level being similar in both groups. The immunosuppressive regimen consisted of anti-thymocyte globulin or baxilisimab in case of high immunological risk, tacrolimus, sirolimus or mycophenolate mofetil and prednisone. Tacrolimus variability was also compared.
The variables of efficacy evaluated were incidence of early graft loss (less than 48 hours), delayed renal function, acute rejection, renal function at 1 and 3 years, patient and graft survival at 1, 3 and 10 years and mean patient and graft survival time.
The results of the variables evaluated were similar in both cohorts.
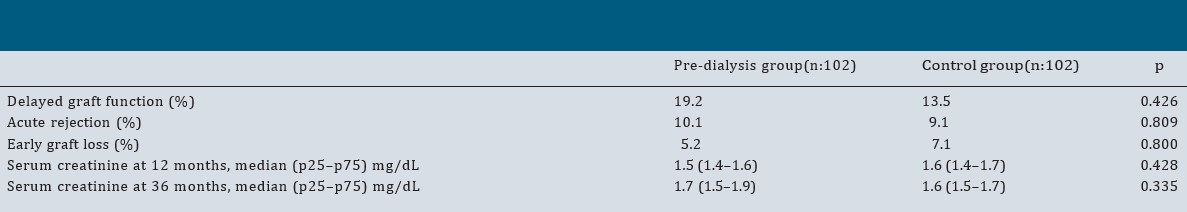
Recipient survival at 1, 3 and 10 years was 94.1% 93.1% and 71.2% in the pre-dialysis group and 96.0% 89,7 and 74.1% in the control group(p = 0.730).
Similarly, graft survival in the pre-dialysis group was 90.4% at one year, 88.1% at 5 years and 62,8% at 10 years, and in the control group it was 92.3% at one year, 79.6% at 5 years and 61,7% at 10 years(p = 0.693).
The mean recipient survival time was similar in the pre-dialysis and control groups (126.8[95%CI:113.8–139.8] vs. 123.1 [95% CI: 109.7–135.5]) months; p = 0.730) Nor were significant differences in the graft survival time observed between the two groups (pre-dialysis group:114.6months[95%CI:99.1–130.2] vs.control group:109.3months [95%CI:93.7–124.8];p=0.693).
Pre-emptive transplant from deceased donors offers outcomes comparable to those of recipients on dialysis and prevents morbidity, mortality and psychological impact derived from dialysis.
[1] renal transplant
[2] pre-emptive transplant
[3] outcome
