
A program of pre-emptive kidney retransplantation from deseased donors
Antonio Franco Esteve1, Patricio Mas Serrano3, Francisco Manuel Marco2, Francisco javier Perez Contreras1.
1Department of nephrology, Hospital Dr Balmis Alicante, Alicante, Spain; 2Department of Immunology, Hospital Dr Balmis Alicante, Alicante, Spain; 3Farmacy, Hospital Dr Balmis Alicante, Alicante, Spain
There is uncertainty about the best approach to replacement treatment for kidney transplant recipients with chronic terminal graft dysfunction, since a retransplant could be performed before resumption of dialysis, thus avoiding this treatment and the dilemma of whether or not to suspend immunosuppressive therapy. However, there is limited experience in pre-emptive - repeat transplantations, and none from deceased donors.
This study aims to assess the results of a pre-emptive - retransplantation program with brain-dead deceased donors.
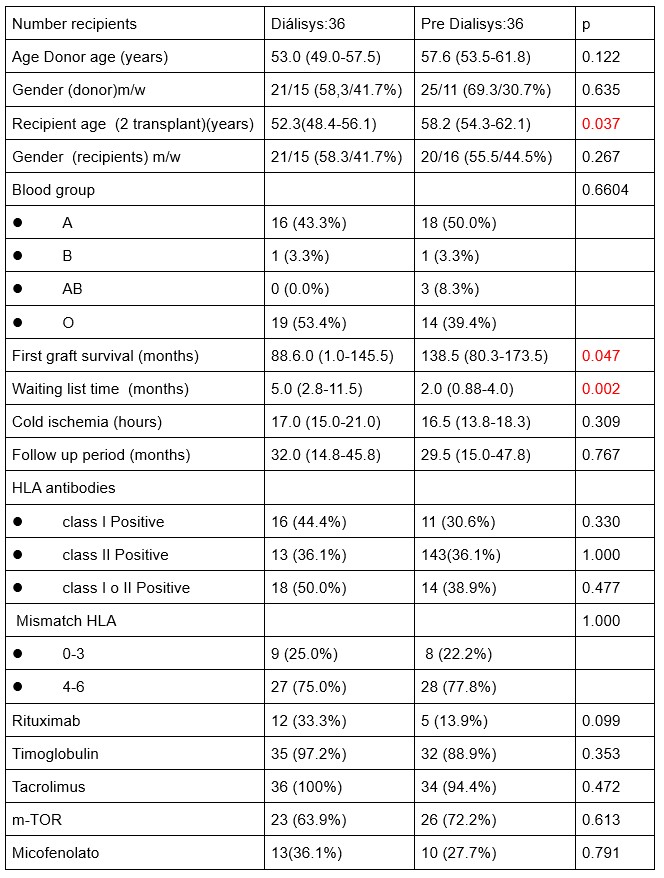
We designed a retrospective matched cohort study, including 36 recipients in the pre-dialysis group and 36 controls who were already on dialysis, matched for donor age and transplant date, which could not differ by more than 7 days between pairs. In the pre-emptive group, patients had to have a glomerular filtration rate less than 15 ml/mn, an estimated time to entry into dialysis of less than 6 months and post-transplant follow up of more than 12 months. We performed pre-emptive transplant only in the event that a candidate already on dialysis was no available for that graft. The immunosuppressive regimen consisted of anti-thymocyte globulin, prolonged release tacrolimus, mycophenolate mofetil or sirolimus, and prednisone. Variables used to standardize the cohorts were donor and recipient age and sex, blood group, duration of the first graft, time on the waitlist to receive the second graft, cold ischemia time, induction and maintenance immunosuppression, and HLA antibodies prior to retransplantation. The efficacy variables were early graft loss, acute rejection, delay in graft function, renal function at the end of follow-up, survival time, and recipient and graft survival at 24 and 48 months’ follow-up.
The pre-dialysis group were older and presented a significantly shorter waitlist time, lower immunization status, and a significantly longer duration of the first graft than the control group.
The percentage of recipients who presented early graft loss, delayed renal function, or acute rejection was similar between groups. No significant differences were observed in kidney function or in the survival of the recipient or graft.
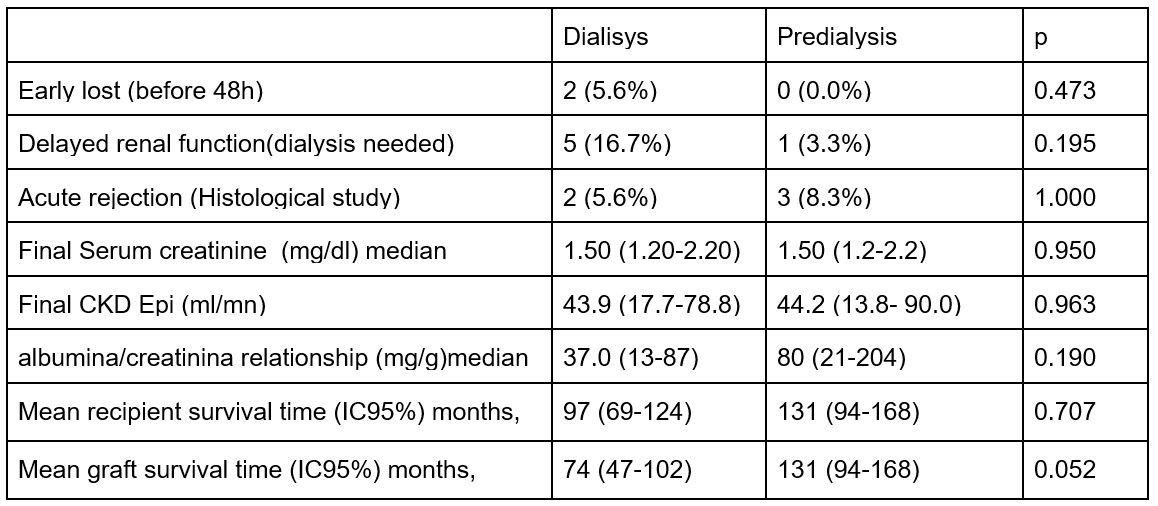
In conclusion, pre-emptive retransplantation from deceased donors yields good outcomes in patients with terminal chronic dysfunction, helping to avoid recurrence to dialysis, shortening the time spent on the waitlist, reducing the risk of producing antibodies, and resolving the dilemma of whether or not to stop immunosuppression.
[1] pre-emptive transplant
[2] deceased donor
[3] waiting list
[4] dialysis
[5] graft survival
[6] patient survival
