
Anti-AT1R auto-antibodies in pancreas transplantation
Christophe Masset1,2, Olivia Rousseau2, Nathalie Gérard2, Nicolas Degauque2, Sophie Brouard2, Magali Giral1,2, Julien Branchereau1,2, Benoit Mesnard1,2, Diego Cantarovich1,2, Jacques Dantal1,2.
1Institut de Transplantation-Urologie-Néphrologie (ITUN), Nantes University Hospital, Nantes, France; 2Center for Research in Transplantation and Translational Immunology, INSERM UMR 1064, Nantes University, Nantes, France
Introduction. Auto-antibodies targeting the angiotensin-II receptor (AT1R-AA) have been identified as drivers of immune response in kidney transplantation, contributing to allograft rejection and early severe arteritis. However, there is limited data on AT1R-AA in pancreas transplant recipients. Therefore, our study aimed to investigate their role in pancreas transplantation, particularly focusing on early pancreatic thrombosis.
Methods. We included all pancreas transplant recipients followed at Nantes University Hospital with available pre-transplant sera between 2000 and 2023. AT1R-AA levels were assessed using standardized ELISA immunoassay on pretransplant sera. The primary outcome was the occurrence of complete pancreatic thrombosis during the first week post-transplantation. Secondary outcomes included pancreas allograft survival at one year and the occurrence of a pancreatic rejection episode. A multivariate cause-specific Cox model was used to examine the association between AT1R-AA and the various outcomes studied. Additionally, pancreatic tissues and arteries from discarded deceased donors were analyzed for AT1R expression to explore potential variations that might explain observed differences.
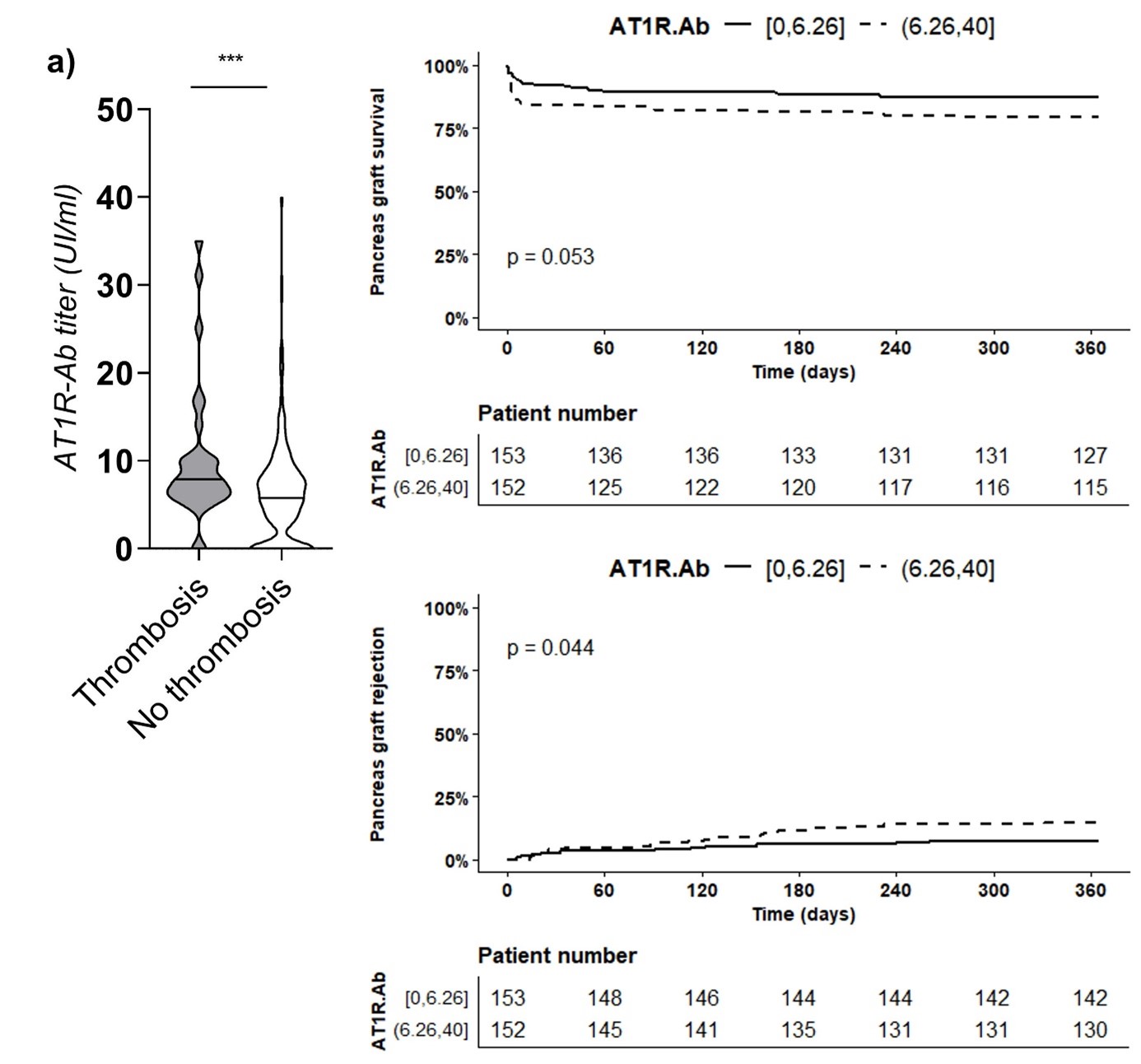
Results. Among the 305 patients included, 32 experienced early pancreatic thrombosis (10.5%). AT1R-AA levels were significantly higher in patients with early thrombosis compared to others (10.1 UI/ml vs 6.3 UI/ml, p < 0.0001). The risk of pancreatic failure during the first week increased with AT1R-AA levels (6.5% vs 14.5% for low vs high titers, respectively, p < 0.01). Pancreas survival at one year was lower in patients with the highest pre-transplant AT1R-AA titers (75% vs 83%, p = 0.05). In multivariate analysis, the presence of AT1R-AA was significantly associated with early allograft failure (HR = 1.05; 95% CI = 1.00; 1.09). Furthermore, AT1R-AA increased the risk of pancreatic rejection (7.2% vs 14.5%, p = 0.04). In the analysis of tissues from discarded donors (n = 21), arterial expression of AT1R was 25% higher among patients treated for hypertension compared to others.
Conclusion. The presence of AT1R-AA was significantly associated with a higher risk of pancreatic failure due to complete thrombosis and an increased risk of pancreas rejection. Variations in AT1R expression related to the donor's condition may contribute to different outcomes observed among patients with pre-transplant AT1R-AA.
This study was supported by institutional grants from the French Society of Diabetes, the French National Agency of Biomedicine and the Foundation for Medical Research.
[1] Anti AT1R autoantibodies
[2] pancreas transplantation
[3] allograft thrombosis
[4] pancreas rejection
