Impact of donor-recipient gender concordance on outcomes following liver transplantation for primary sclerosing cholangitis
Shiva Kumar1, Songhua Lin2, Jesse D Schold3.
1Dept. of Gastroenterology & Hepatology, Cleveland Clinic Abu Dhabi, Abu Dhabi, United Arab Emirates; 2Quantitative Health Sciences, Cleveland Clinic Foundation, Cleveland, OH, United States; 3Depts. of Surgery & Epidemiology, University of Colorado Anschutz Medical Campus, Aurora, CO, United States
Introduction: Even though donor and recipient gender have been shown to potentially impact outcomes following liver transplantation (LT) in Primary Sclerosing Cholangitis (PSC), limited data exist regarding impact of gender and donor-recipient gender concordance. Our aim was to evaluate impact of donor and recipient gender and their concordance on outcomes following LT in PSC.
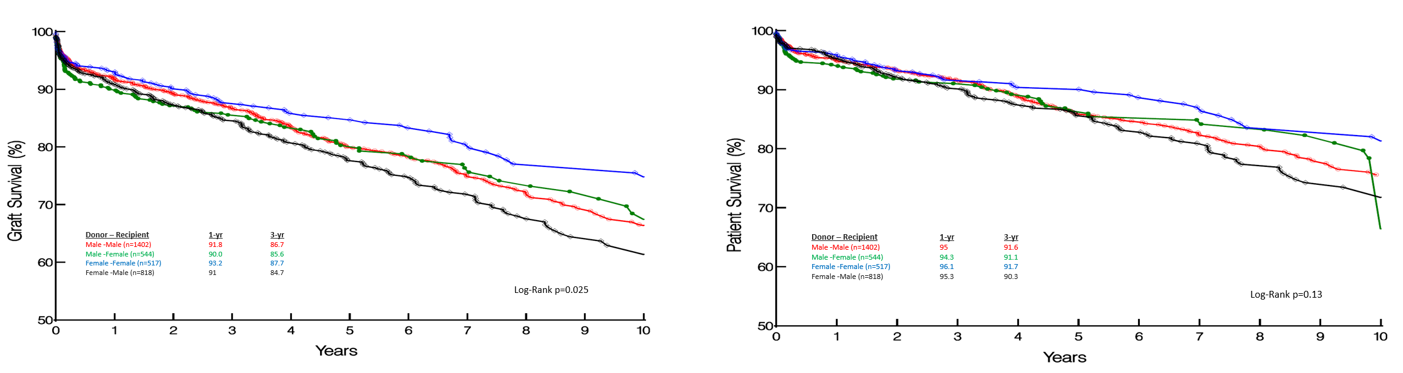
Methods: Using the Scientific Registry of Transplant Recipients (SRTR) we constructed a retrospective cohort of recipients undergoing primary LT for PSC between Jan 2010-Dec 2021, stratified by recipient and donor gender: Male-Male (M-M), Male-Female (M-F), Female-Male (F-M) and Female-Female (F-F). Primary outcome measures were graft and patient survival. Survival comparison was performed using the Kaplan-Meier method with log-rank test and multivariable analysis of outcomes using Cox proportional hazard models.
Results: 3281 recipients with PSC underwent LT over the study period: M-M: 1402 (42.7%), M-F: 544 (16.5%), F-M: 517 (15.8%) and F-F: 818 (25%). While recipient age was comparable among study cohorts, female donors were older (M-M vs. M-F vs. F-M vs. F-F: 38.3 vs. 37.9 vs. 42.7 vs 43.8; p<0.0001). While recipient BMI was lower in F-F (p=0.03), donor BMI was higher (p<0.0001). Greater proportion of donation after circulatory death (DCD) donors were male (M-M 6%, M-F 6.4%, F-M 3.3%, F-F 3.1%; p<0.0001), while female recipients were more likely to undergo living donor LT (LDLT) (M-M 4.3%, M-F 8.6%, F-M 5%, F-F 6%; p<0.0001). The four study cohorts were comparable with respect to all other variables including cold ischemia time.
1- and 3- year graft survival was superior when recipient and donor were of the same gender (1 Yr GS: M-M 91.8%, M-F 90%, F-M 91%, F-F 93.2%; p=0.02) (3 Yr GS: M-M 86.7%, M-F 85.6%, F-M 84.7%, F-F 87.7%; p=0.02). A similar trend was observed with patient survival, but this did not reach statistical significance (p=0.13). Overall, despite higher age and BMI of female donors, short- and long-term graft and patient survival were highest among female recipients of grafts from female donors (Graft survival: 1 Yr: 93.2, 3 Yr: 87.7; Patient survival: 1 Yr: 96.1, 3 Yr: 91.7). On multivariable analysis, while recipient female gender and F-F were associated with favorable graft (p=0.0002, p=0.005) and patient survival (p=0.002, p<0.0001), DCD status and cold ischemia time were associated with inferior outcomes.
Conclusions: Majority of recipients with PSC undergoing DDLT in the US receive grafts from male donors, while female recipients are more likely to undergo LDLT. Graft survival was superior among female recipients and in cohorts with donor-recipient gender concordance, with female recipients of grafts from female donors having the best outcomes. Further study is needed to help understand the mechanisms underlying this observation. Consideration of donor-recipient gender concordance may help optimize outcomes in recipients with PSC undergoing LT.
[1] Gender
[2] Primary Sclerosing Cholangitis
[3] Allograft Survival
[4] Liver Transplantation
