
Dynamic trends in deceased donor kidney utilization: Unraveling discard rates and KDPI shifts across pre-COVID, COVID, and post-COVID eras
Rachael E Ketcham1, Ronald A Squires1, Jeff G Mathews1, Clint A Hostetler1, Jeffrey P Orlowski1.
1LifeShare Network, Inc., Oklahoma City, OK, United States
Purpose: This study aims to investigate trends in deceased donor kidney (DDK) utilization over a five-year period at a single OPO. By comparing Pre-COVID (PRE), COVID, and Post-COVID (POST) periods, we aim to discern any significant shifts in DDK transplantation patterns. A key focus is placed on understanding whether the observed increase in discard rates is associated with a decline in organ quality, by evaluating KDPI values of the donors.
Methods: We collected data from our internal electronic medical record on DDK discards, transplants, and KDPI from PRE, COVID, and POST eras. The study spans January 1, 2018 – October 31, 2023, examining 385 PRE, 447 COVID, and 433 POST donors. Statistical analyses were performed to assess the significance of observed trends and differences.
Results: Over the five-year period (2018-2023), the total number of deceased donors increased steadily, reaching 249 in 2022, with a projected total of 233 in 2023. Notably, DCD donors exhibited strong growth (+70.6%), from PRE (137) to projected POST (234). Recovered brain dead donors have held consistent when comparing PRE (248) with projected POST (248). The total number of donors has increased across the three eras, from PRE to COVID (+16.1%), COVID to projected POST (7.8%) and comparing POST to PRE (+25.2%). Discard rates demonstrated an upward trajectory, with PRE, COVID, and POST rates at 22.57%, 24.52%, and 28.92%, respectively (Figure 1).
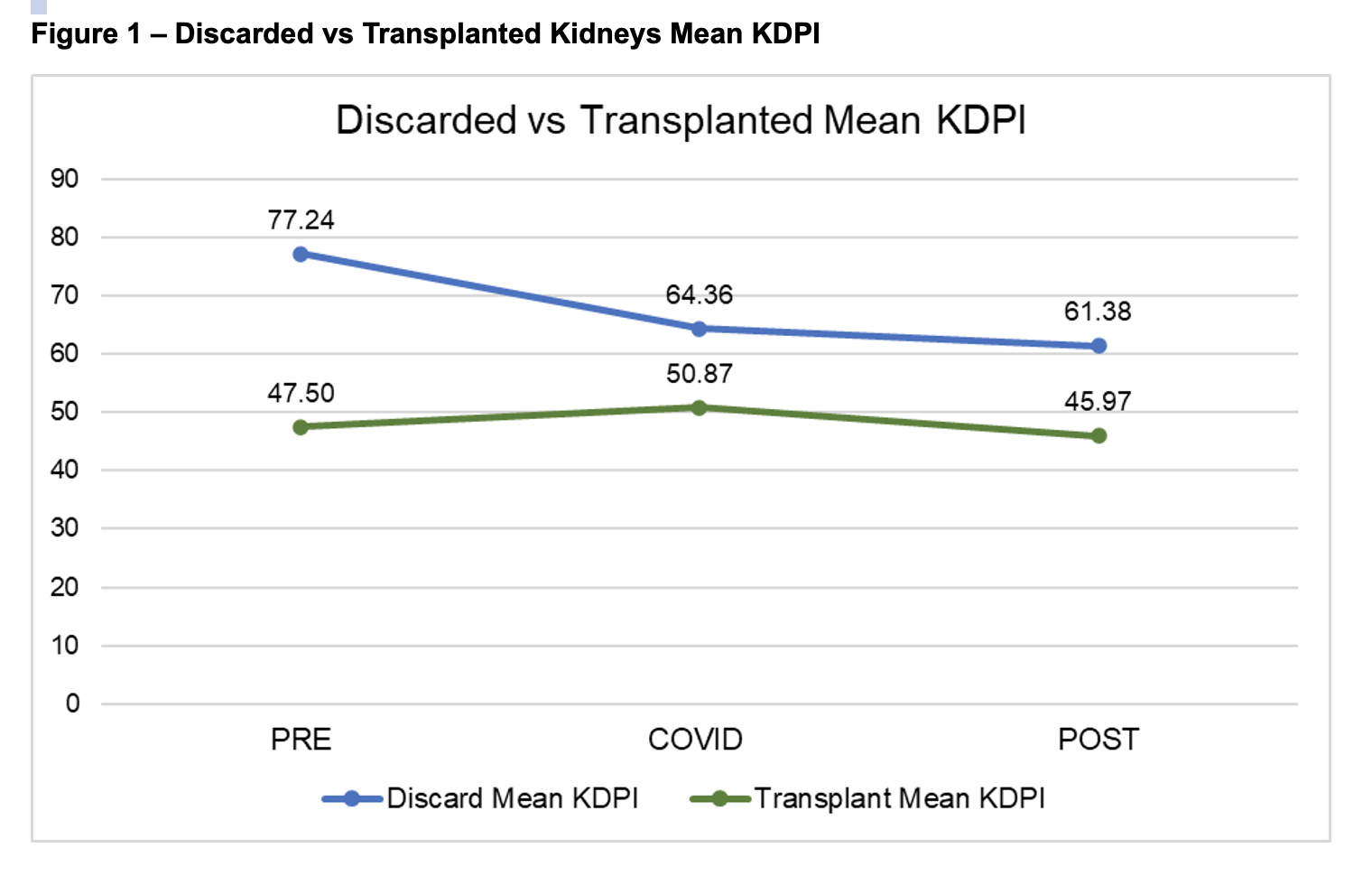
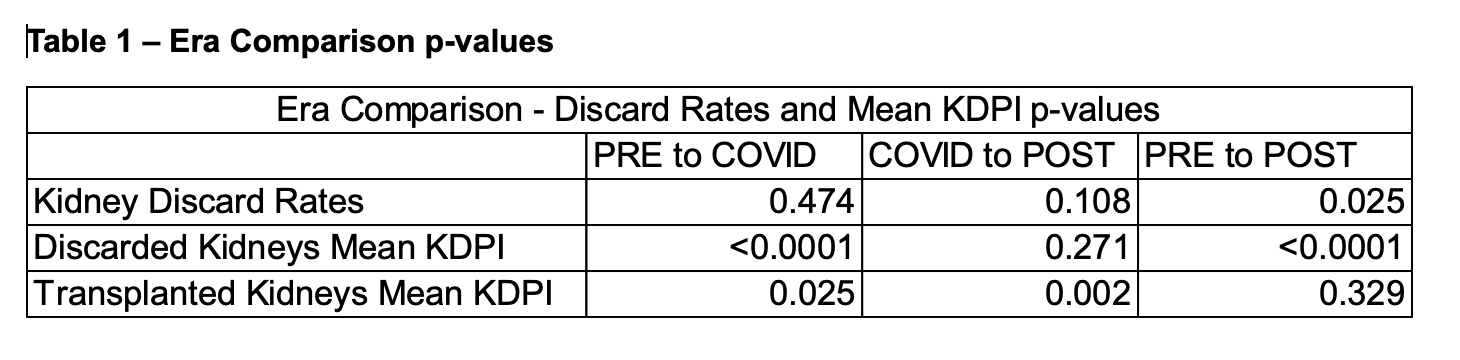
Discard rates during the POST era demonstrated a significant increase compared to PRE (p = 0.025) (Table 1). Examining KDPI values indicated differences in mean values for both discarded and transplanted DDK. The mean KDPI for discarded DDK during the COVID (64.36) and POST eras (61.38) were both significantly lower (p <0.0001) than that of the PRE (77.24) (Table 1). Interestingly, no significant difference was observed between COVID and POST discard mean KDPIs (p = 0.271). Additionally, mean KDPI values for transplanted donors demonstrated variations: PRE (47.50), COVID (50.87), POST (45.97). PRE to COVID transplant KDPIs indicated significant differences (p = 0.025), as did COVID to POST (p = 0.002) (Table 1).
Conclusions: The study provides valuable insights into DDK utilization patterns, highlighting a growing trend in DCD donors and an increase in discard rates. Contrary to expectations, the mean KDPI did not worsen, indicating that the observed discard rate escalation may be attributed to increased selectivity rather than a decline in organ quality. This study underscores the importance of assessing not only discard rates but also the quality of discarded organs to better understand the dynamics of DDK utilization. Further research is warranted to explore the nuanced factors influencing transplant center acceptance patterns in the context of evolving organ procurement and allocation strategies.
