
An Inconvenient Offer: A Single OPOs Experience in Kidney Utilization
Rachael E Ketcham1, Jeff G Mathews1, Ronald A Squires1, Clint A Hostetler1, Jeffrey P Orlowski1.
1LifeShare Network, Inc., Oklahoma City, OK, United States
Purpose: The purpose of this study was to examine our OPO’s kidney utilization experience as a leader in DCD donors. As our count of recovered donors climbed, so did our kidney discard rate. We sought to understand the key influences causing this trend.
Methods: Data were obtained from our internal electronic medical record. Recovery dispositions for 2,478 deceased donor kidneys (DDK) recovered with intent to transplant were examined for the time period of January 1, 2018 - October 31, 2023. We organized two sub-groups for year-over-year comparison based on the day of the week of recovery: Monday-Thursday/non-holiday (Weekday) and Holiday/Friday-Sunday (Weekend). Due to the COVID pandemic occurring during our study period, we also performed a pre-COVID, COVID & post-COVID period comparison. Chi-squared testing and two proportion z-tests were utilized to compare counts of observed and expected discards and discard rates between the cohorts, respectively. We evaluated mean KDPI from year-to-year to understand donor quality trends.
Results: The study consisted of 1,275 deceased renal donors, of which 558 were DCDs. Using projected values for 2023, analysis revealed 24% growth in recovered renal donors and 17% in DDK transplants. This was primarily due to an increase of DCD donors (+85%) and DDK transplanted (+65%). Compared to 2018, there were decreases in 2023 for BD renal donors (–3%) and transplants (–2%). Additionally, 43.5% of DDK recovered with intent were in the Weekend cohort. The Weekend cohort also had 49.3% of the total DDK discards. Discard rates increased year-over-year for both cohorts (Figure 1) with averages of 22.9% for the Weekday, and 28.8% for the Weekend cohorts.
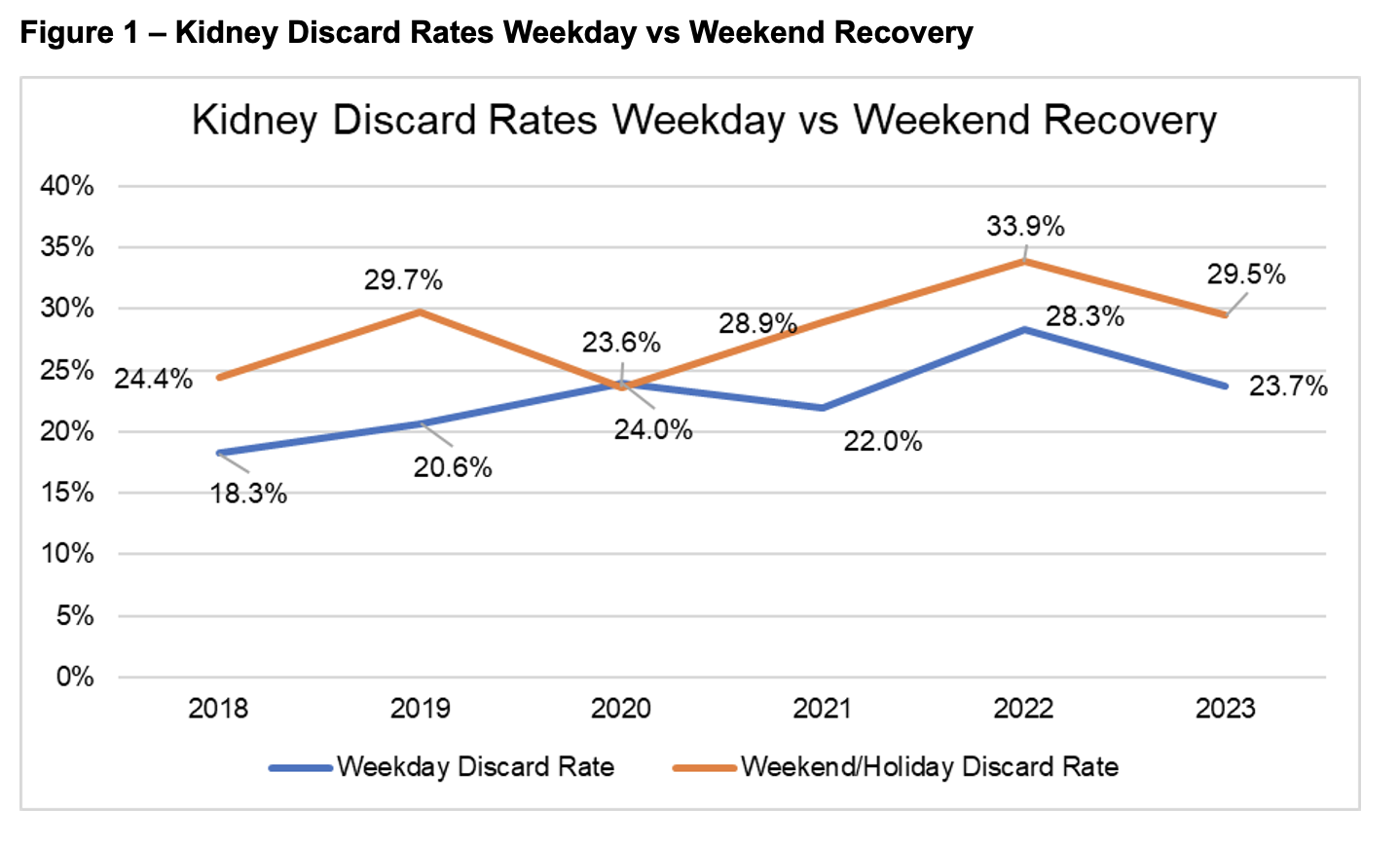
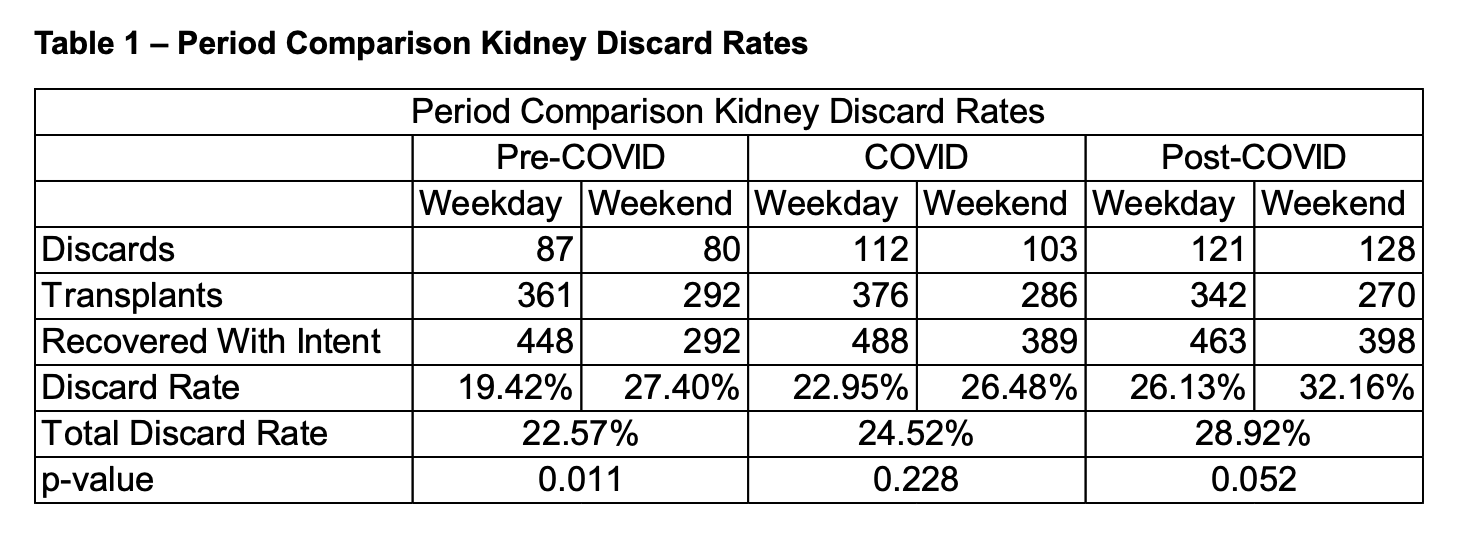
Chi-squared testing indicated significant differences in kidneys discarded year-over-year between the two cohorts (p = 0.011). The z-tests indicated significant differences between discard rates for cohorts in the pre-COVID (p = 0.011) and post-COVID (p = 0.052) periods, but not the COVID period (p = 0.228) (Table 1).
Compared to 2018, mean KDPI in 2023 decreased for donors with discards (–6%, p = 0.202), donors with transplants (–11%, p = 0.071) and all donors combined (–9%, p = 0.076).
Conclusions: Kidneys from DCD donors are known to have satisfactory outcomes post-transplant. However, transplant centers frequently refuse DDK offers, and annually, nearly 30% DDK are not used, often due to being recovered from a DCD donor and recovery timing. Because the BD donor pool isn’t expanding, increased utilization of DCD kidneys is imperative to reaching our collective goals of increasing deceased donor transplants and decreasing waitlist times. Given the observed trends in kidney discard rates and the evolving dynamics of DCD donor utilization, further research is warranted to explore targeted strategies for optimizing DDK acceptance and utilization.
