Identification of risk of malaria and selective post-transplant testing of deceased organ donors in the UK
Ines Ushiro-Lumb1, Christie Geoghegan1, Marita Smit1, Ruwanika Kothalawala1, Victoria Maddox1, Mhairi Webster1.
1NHS Blood and Transplant, London, United Kingdom
Background: Besides the traditional set of infectious markers applied during donor assessment, such as some of the blood-borne viruses, additional screening may be required when specific risks are identified. Demographics and epidemiological details help inform the risk of geographically-restricted, asymptomatic infections in potential organ donors. Transmission of donor-derived malaria through organ transplantation has been well described and can hold high morbidity and mortality, mainly due to late recognition. It is an uncommon event in non-endemic countries but more importantly, risks can be mitigated through awareness, early diagnosis and appropriate treatment.
Aim: Inform the basis for post-transplant selective testing of deceased donors, and raise awareness of existing processes, criteria for testing and relevance to the safety of organ donation and transplantation. Summarise the results obtained since introduction of discretionary post-donation malaria testing for deceased organ donors in the UK.
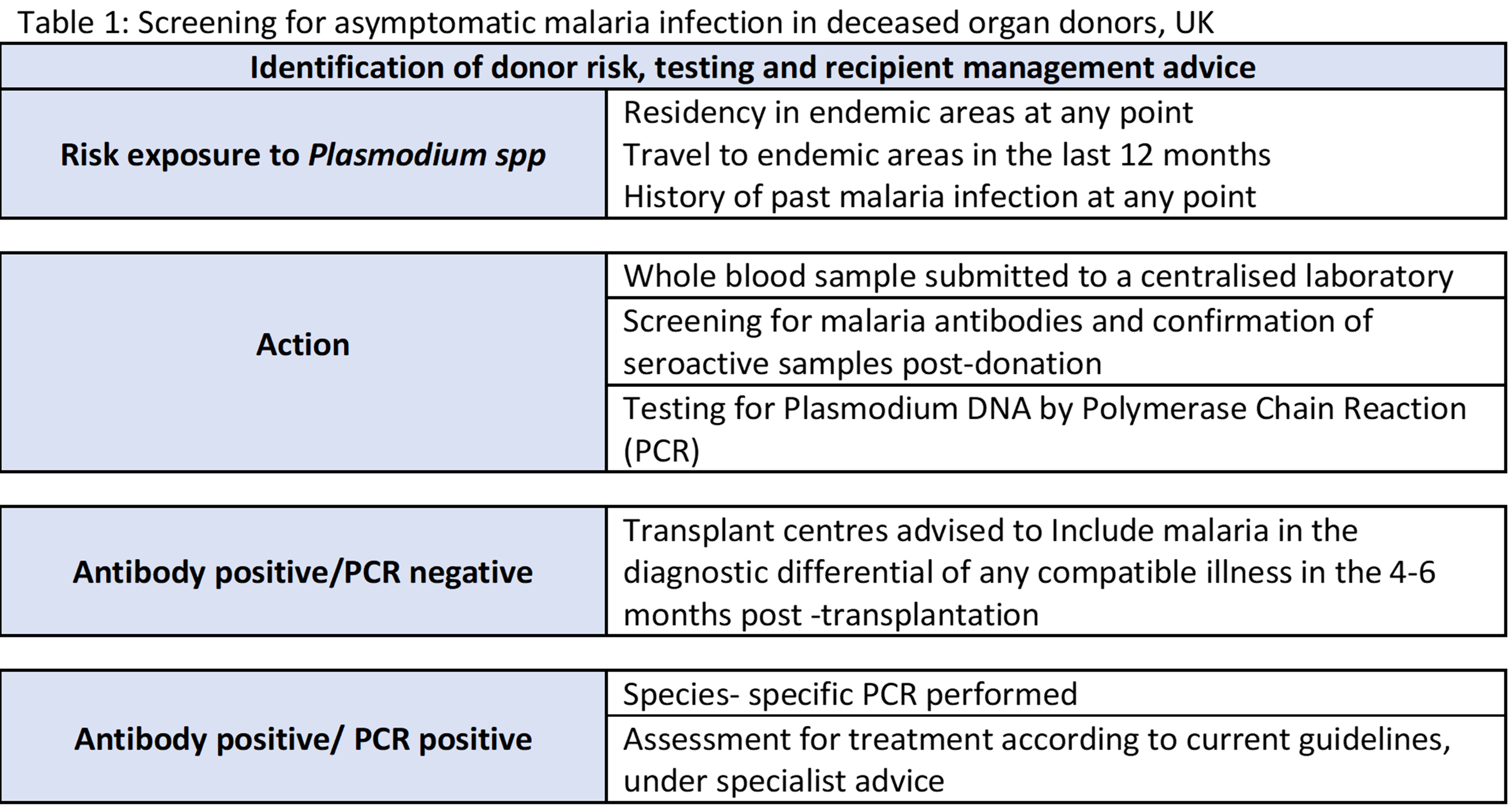
Methods: Criteria applied for post-donation testing of selected donors for asymptomatic infection is shown in Table 1. Testing pathway and communication to transplant centres is also shown in Table 1. Testing is done centrally in a reference laboratory, with results available within the first week following transplantation. Significant results are actively communicated to transplant centres.
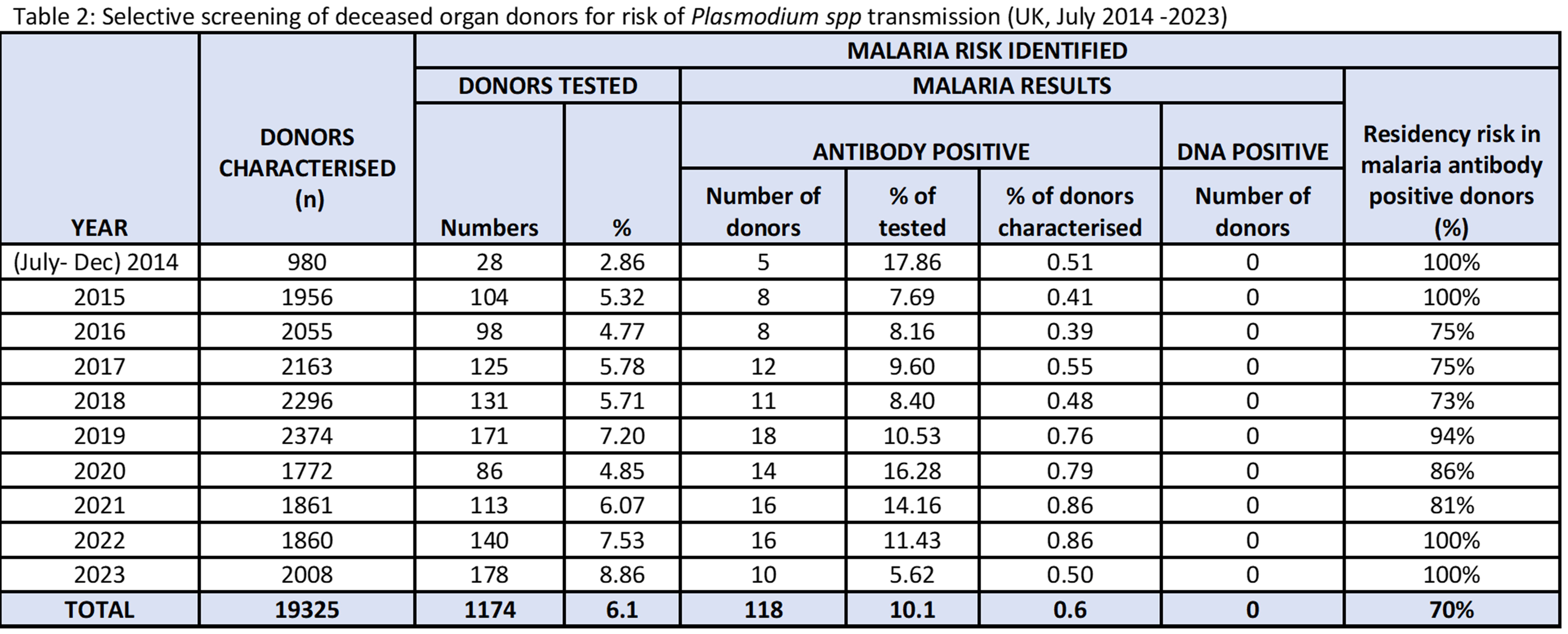
Results: Between 2014 and 2023, approximately 19,325 potential deceased organ donors were routinely screened for microbiological markers; 6.1% had identifiable risk factors and for malaria (n= 1174), with 10% of those testing positive for malaria antibodies. No donor had detectable Plasmodium spp DNA detected in whole blood. Antibody positivity is mainly observed in individuals who were born and resided in malaria endemic areas; Table 2 summarises our findings.
Discussion: In organ donation, a balanced risk-benefit assessment, local epidemiology of infection, availability of reliable screening tools and of effective prophylaxis or treatment are some of the parameters used to guide the best way to mitigate harm to transplant recipients. In the UK, as a non-endemic area for many relevant geographically restricted infections, post-transplant testing offers the possibility of monitoring and intervention, without compromising organ acceptance. In the case of malaria, the transmission risk comes from semi-immune individuals who may have low levels of parasitaemia and no symptoms at the point of donation; the risk is highest from individuals who have resided in endemic areas and it remains even many years after they have left these areas. No cases of malaria transmission via solid organ transplantation have been described in the UK. Strategies must be aligned to local needs and should be continuously monitored. Should the epidemiology of these infections change, resulting in different levels of risk, processes will need to be adapted accordingly.
[1] Malaria
[2] Donor Screening
[3] Deceased Donor
[4] Donor Characterization
[5] Selective Testing
[6] Risk Mitigation
[7] Malaria semi-immunity
[8] Geographically-restricted infection
