
A virtual community assertive treatment model for organ donor family aftercare in the United States
Macey Levan1, Samantha Klitenic1, Jasmine Ahktar1, Carolyn Sidoti 1, Tara Storch3, Elizabeth Hughes3, Steven Wall 1, Tessa Flower 2, Tara Kane2, Paige Anderson3, Hannah Showalter 3, Brittany Koons4.
1Surgery, NYU Langone Health , New York, NY, United States; 2Aftercare, Infinite Legacy , Baltimore, MD, United States; 3Taylor's Gift Foundation , Coppell , TX, United States; 4M. Louise Fitzpatrick College of Nursing , Villanova University , Philadelphia , PA, United States
Introduction: There is variation in aftercare support services provided by geographically diverse and federally designated organ procurement organizations (OPOs) in the United States. In an effort to better serve donor families, a donor family led non-profit developed a novel, virtual aftercare program using the evidence-based assertive community treatment model. The program pairs participants with a certified peer-coach ('Caring Guide') trained in an organ donation specific grief-topic curricullum, and organizes loss-specific facilitated support groups. We evaluated participant and OPO staff experiences with the program, to gain a better understanding of acceptability and adoption at an OPO-level and to evaluate impact on grief symptom trajectory and perceived social support.
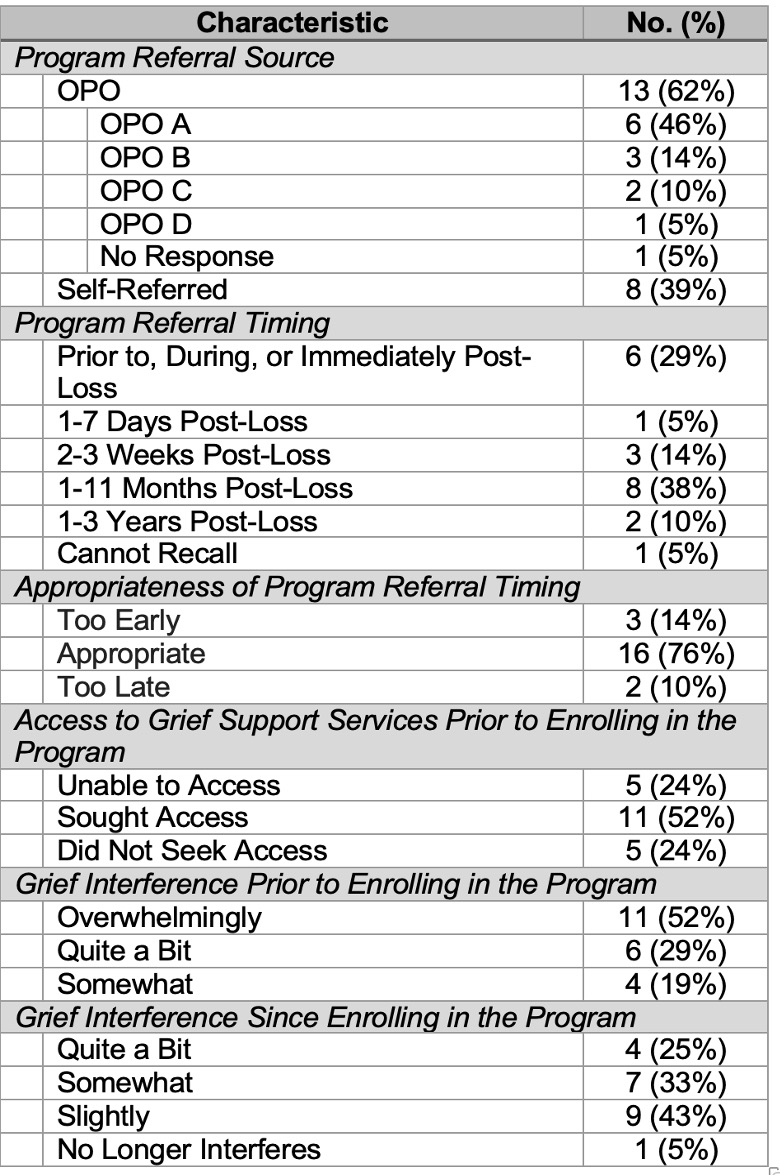
Methods: Investigators conducted semi-structured interviews with 21 program participants and 6 OPO staff members. Questions assessed referral process, source, timing, and appropriateness of the referral, access to grief support and/or mental health services prior to enrollment in the program, program resource(s) utilized, change in grief symptoms, and suggestions for improvement. Results were analyzed using both rapid qualitative analysis and descriptive statistics.
Results: Referral timing varied significantly across OPOs and ranged from hours pre-loss to years post-loss (Table 1). Barriers to referral and enrollment were difficulty reaching families, determining if the program received an OPO's referral, scheduling conflicts, and communicating with non-English and non-Spanish speakers. All OPO staff members reported working with families without access to mental health services. 52% of participants reported struggling to access mental health services. Eighteen (86%) participants worked with caring guides, while 12 (57%) attended an average of 7 support groups. Participants valued highly their caring guides’ compassion, support, and empathy, and cited having someone to talk/relate to, connecting with others, and feeling supported as what they liked about the program. 86% of participants reported a decrease in grief intensity since enrolling in the program. Of the 19 participants who experienced anxiety symptoms and the 17 who experienced depressive symptoms, 15 (79%) reported a decrease in anxiety symptoms and 13 (76%) reported a decrease in depressive symptoms since enrolling in the program.
Conclusions: Effective aftercare services are imperative for donor families as a means of coping with, and adapting to, their loss. This novel aftercare program enabled donor families to access otherwise inaccessible grief support services and provided a valuable means of social support. Future research and pragmatic clinical trials should assess efficacy and work through barriers to referral and enrollment.
[1] organ donation
[2] ethics
[3] organ procurement
[4] psychosocial
