
Utilisation of livers donated after circulatory death (DCD) for transplantation – a large cohort study evaluating pre-retrieval biochemical characteristics and transplant outcomes
Syed Hussain Abbas1, Sadr Shaheed1, Letizia Lo Faro1, Fungai Dengu1, Carlo Ceresa3, Alireza Morovat4, Simon Knight1, Leanne Hodson2, Quin Wills5, Rutger Ploeg1, Peter Friend1.
1Nuffield Department of Surgical Sciences, University of Oxford, Oxford, United Kingdom; 2Nuffield Department of Medicine, University of Oxford, Oxford, United Kingdom; 3Liver Transplant Unit , Royal Free Hospital, London, United Kingdom; 4Department of Biochemistry, John Radcliffe Hospital, Oxford, United Kingdom; 5OchreBio Ltd., Oxford Science Park, Oxford, United Kingdom
Background: Donation after circulatory death (DCD) livers are at risk of primary non-function (PNF) and intra-hepatic-biliary stricture formation. The risk of these complications has greatly inhibited the utilisation of DCD livers. This study aims to identify pre-retrieval biochemical characteristics of DCD donors and evaluate the impact of DCD status on organ retrieval, utilisation and graft/recipient outcome.
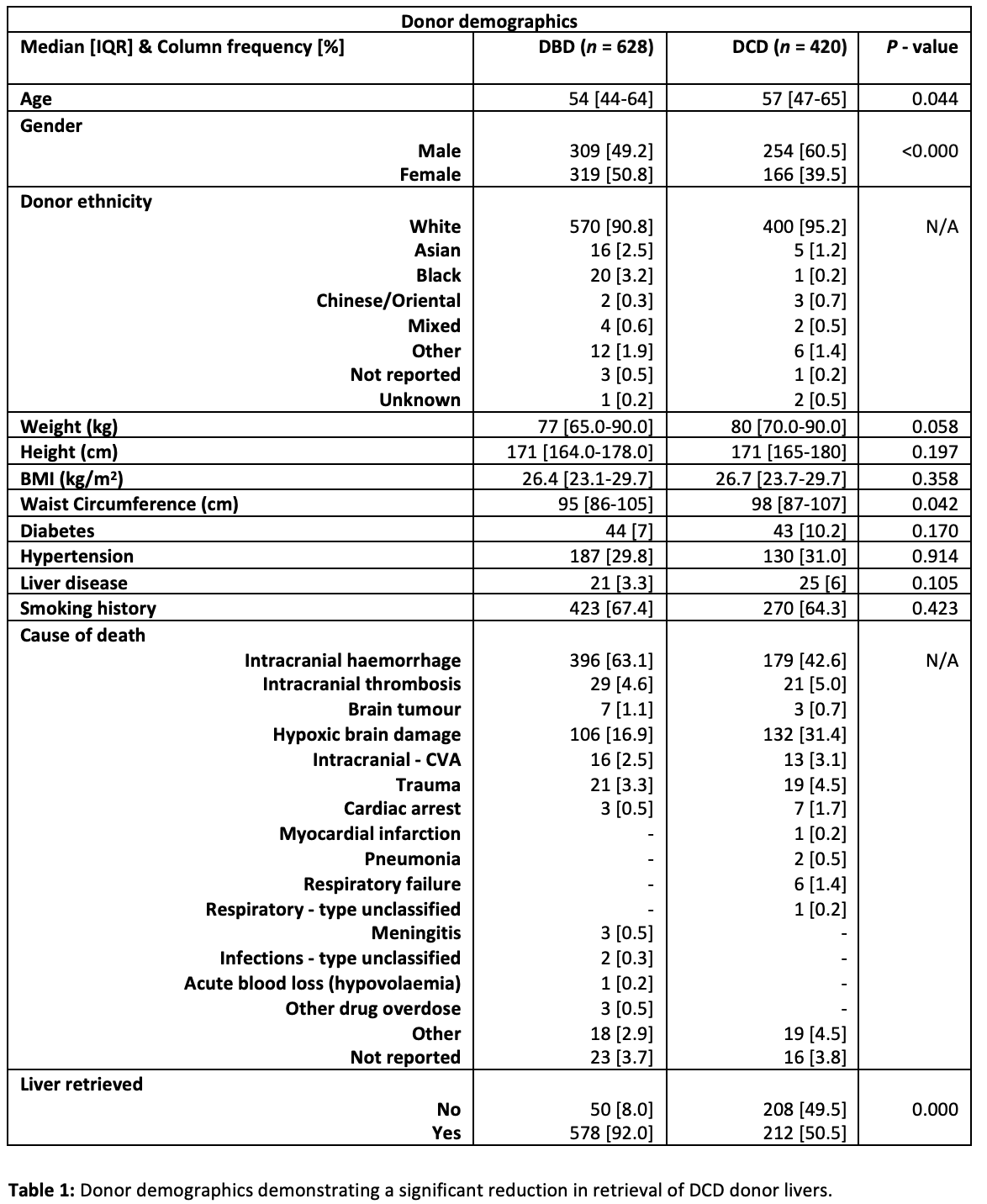
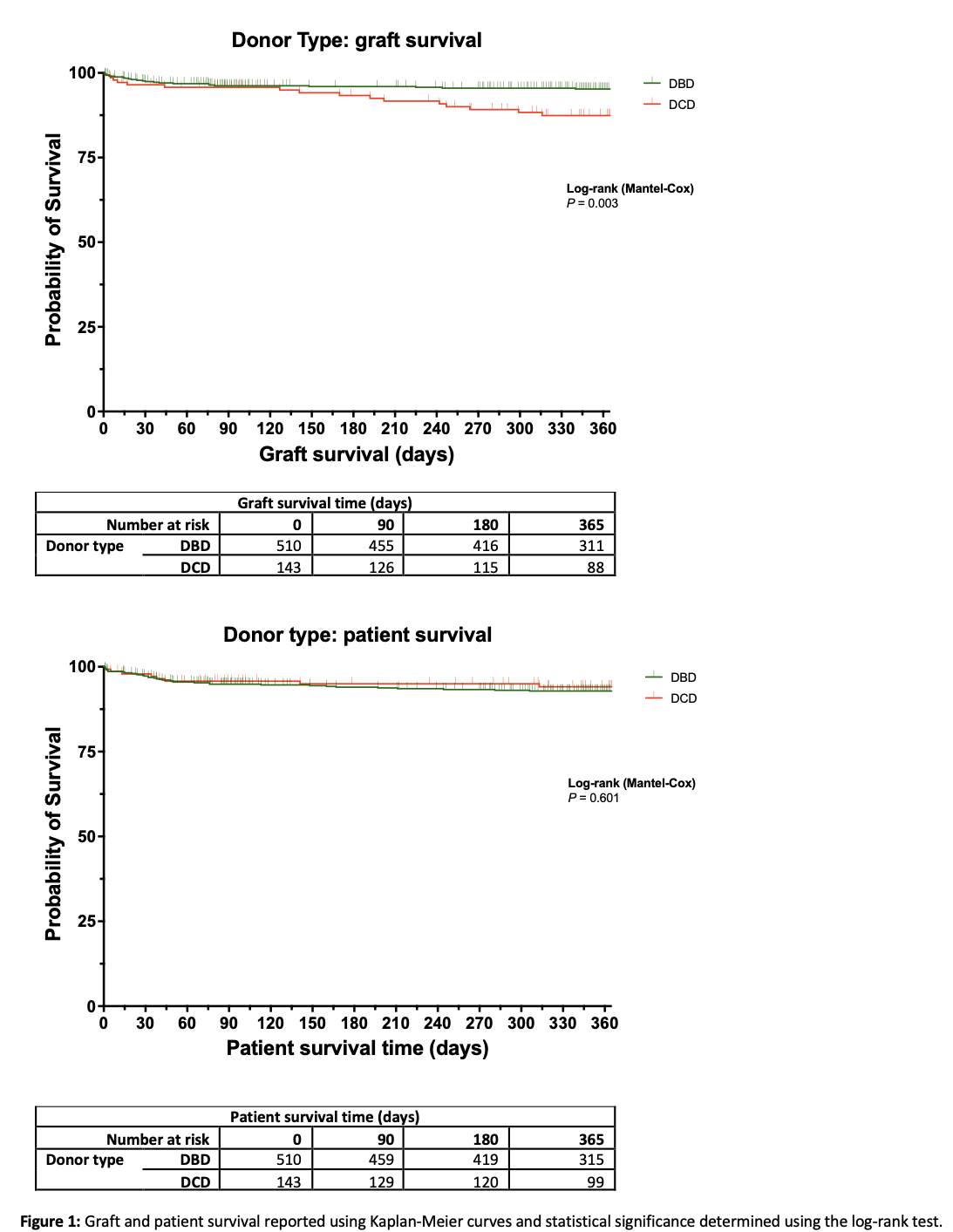
Methods: A total of 1,048 consecutive donors (DBD n=628; and DCD n=420) between 2017-2019 were identified from the national Quality in Organ Donation (QUOD) bioresource and were included in this study. Donor blood collected prior to retrieval was requested for biochemical analysis. The Chi-square test was used for categorical data and the non-parametric Kruskal-Wallis test was used for continuous data. Graft and patient survival were reported using Kaplan-Meier curves.
Results: Pre-retrieval biochemical measurements demonstrated greater hepatocellular injury and metabolic derangement in DCD compared to DBD donors (P<0.001): ALT=38 IU/L (20.1-70.4) vs. 26.9 (16.2-57.5); AST=50.8 IU/L (28.0-83.6) vs. 29.9 (18.4-53.5) and; GGT=71.3 IU/L (30.8-177.2) vs. 40.1 (21.7-88.3), Glucose=6.3 mmol/l (5.1-7.9) vs. 8.2 (6.6-10.0) and; Insulin=84.7 pmol/l (47.0-157.7) vs. 185.6 (89.1-404.6). Only 212/420 (50.5%) of DCD livers compared to 578/628 (92%) of DBD livers were retrieved (Table 1), and of these, only 143/212 (67.5%) of DCD livers and 510/578 (88.2%) of DBD livers were transplanted, P<0.001. Recipients transplanted with DCD livers had a higher rate of biliary strictures i.e. 9.1% vs. 5.5% and significantly reduced graft survival at 12-months i.e. 88.8% vs. 95.5%, P=0.003 (Figure 1). Cox proportional hazard regression analysis identified DCD donors and donor insulin as independent predictors of graft survival.
Conclusion: This study highlights the under-utilisation of DCD livers and identifies pre-retrieval biochemical/metabolic derangements that contribute to risk profile of these donors. The clinical application of normothermic regional perfusion (NRP) and ex-situ machine perfusion technologies may enable donor liver functional assessment/optimisation in order to facilitate safe transplantation.
[1] DCD
[2] Liver Transplant
