Octreotide: Bursting the bubble of lymphoceles in renal transplant recipients
Syeda Hurmath1, Rajeevalochana Parthasarathy1, Sanjeev Nair1, Veena Manjari1.
1Nephrology, Madras medical mission hospital , Chennai, India
Background: Lymphoceles and lymphorrhea are well known lymphatic complications in renal transplant patients. It occurs predominantly in the first 12 weeks following transplantation. Mostly, these are small and insignificant, but large lymphoceles may cause symptoms like pain abdomen, infection, deterioration of graft function, fever, compressive syndrome of the venacava or portal vein. Iliac vessel injuries during surgery, damage to the allograft hilum, unligated recipient iliac lymphatics draining directly from the renal allograft are some of the theories for lymphocele formation. Therapeutic options include laparoscopic/open surgical or percutaneous drainage, with each having different profiles of efficacy and complications. Octreotide has been reported to be an effective treatment for lymphorrhea after axillary lymphadenopathy . We report 3 cases of symptomatic lymphoceles post renal transplant managed with octreotide at our center.
Case 1
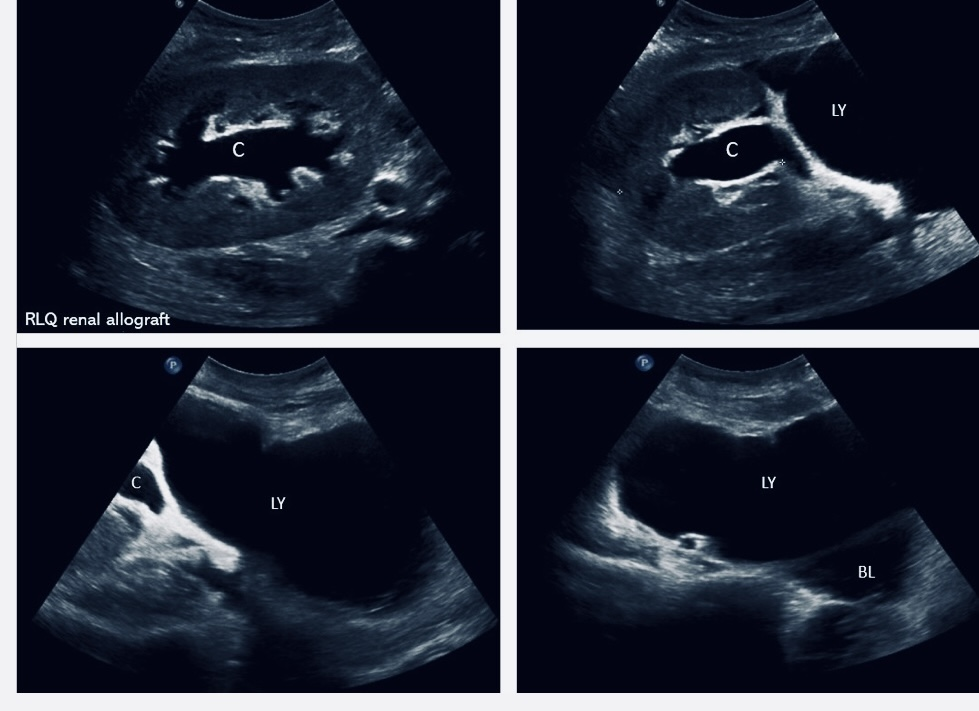
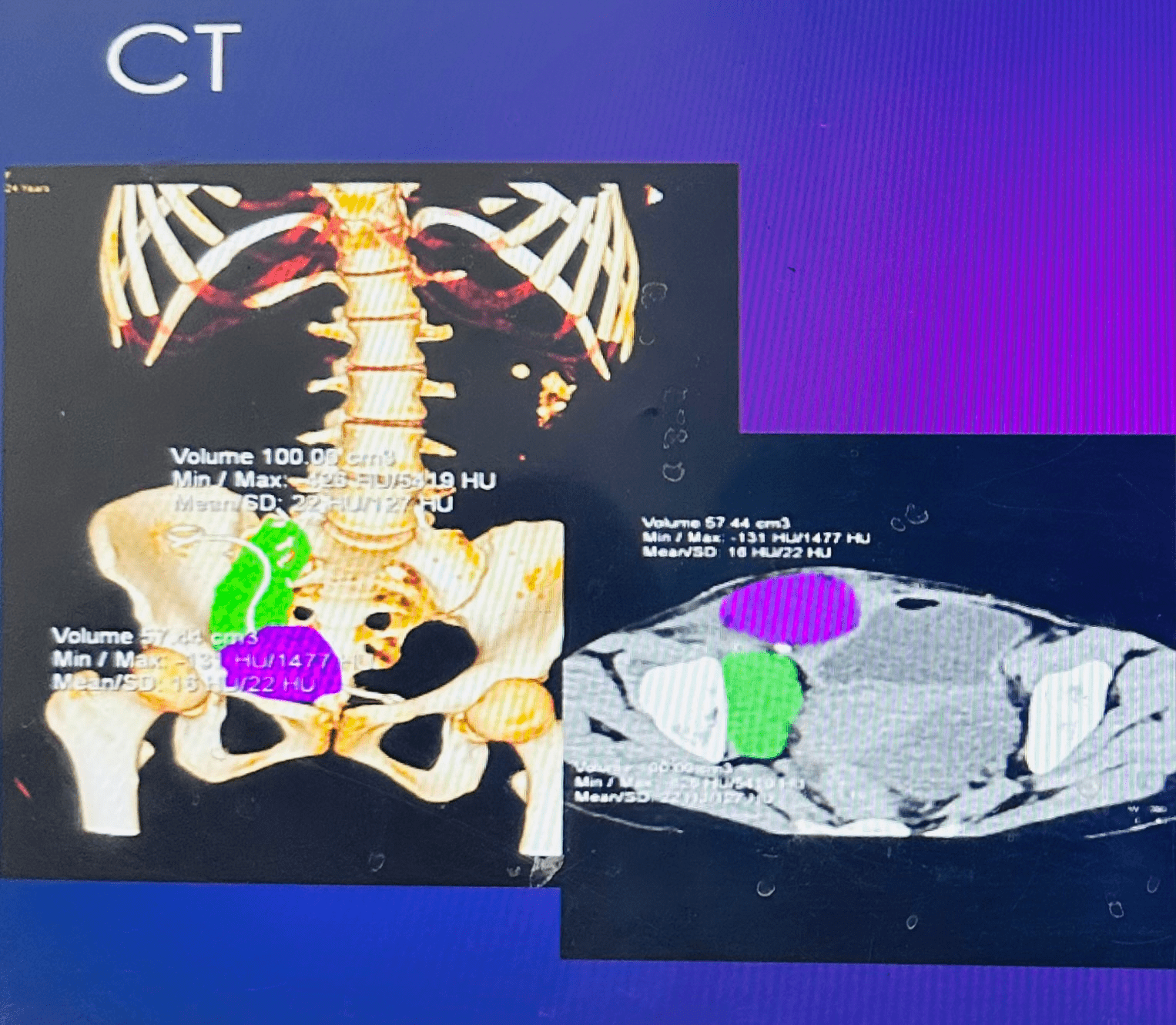
24 year female 3 weeks post renal transplant developed mild graft dysfunction and low grade fever. Imaging showed a large collection abutting the transplant ureter both anteriorly and posteriorly, pig tail insertion was done. Drain output was more than 3 litres per day.
Case 2
56 year old male developed abdominal distension and pain 4 days after renal transplant. Drain output was more than half a litre per day.
Case 3
53 year old male 15 days post renal transplant presented with graft dysfunction. USG revealed collection near lower pole of the kidney with mild hydroureteronephrosis. Drain output was 110 ml.
All 3 cases were treated with 20 mg of intra muscular octreotide. There was significant decrease in drain output with radiological shrinkage in the size and there was no recurrence of lymphocele on follow up.
Conclusion: In kidney transplant patients, lymphoceles still remain a surgical complication due to dissection of the lymphatics of the recipients and the graft. Depot preparation of intramuscular octreotide may be a potential treatment armamentarium for large symptomatic lymphocele post kidney transplant.
[1] Lymphocele
[2] Renal transplant
[3] Surgical complication
[4] Intramuscular octreotide
[5] Lymphorrhea
