Beyond barriers: Navigating the transplant terrain with pre transplant dsa using low dose desensitisation protocol in live donor renal transplantation
Syeda Hurmath1, Rajeevalochana Parathasarathy 1, Sanjeev Nair1, Veena Manjari1.
1Nephrology , Madras Medical Mission hospital, Chennai, India
Introduction: Given the current organ scarcity, living donor kidney transplantation is increasingly performed across HLA or ABO antibodies barrier. It is controversial whether all pre transplant donor specific antibodies detected by the solid phase single antigen bead (SAB) assay negatively affect kidney transplantation outcomes.
The objectives of our study include:
1. Investigating whether the presence of pre transplant DSAs (Donor Specific Antibodies) correlate with higher rates of rejection, graft failure, or other adverse outcomes post transplant.
2. Assessing the effectiveness of low dose desensitisation protocol in improving transplant outcomes for sensitised patients.
The study aims to provide valuable insights into the clinical relevance of pre- transplant DSAs.
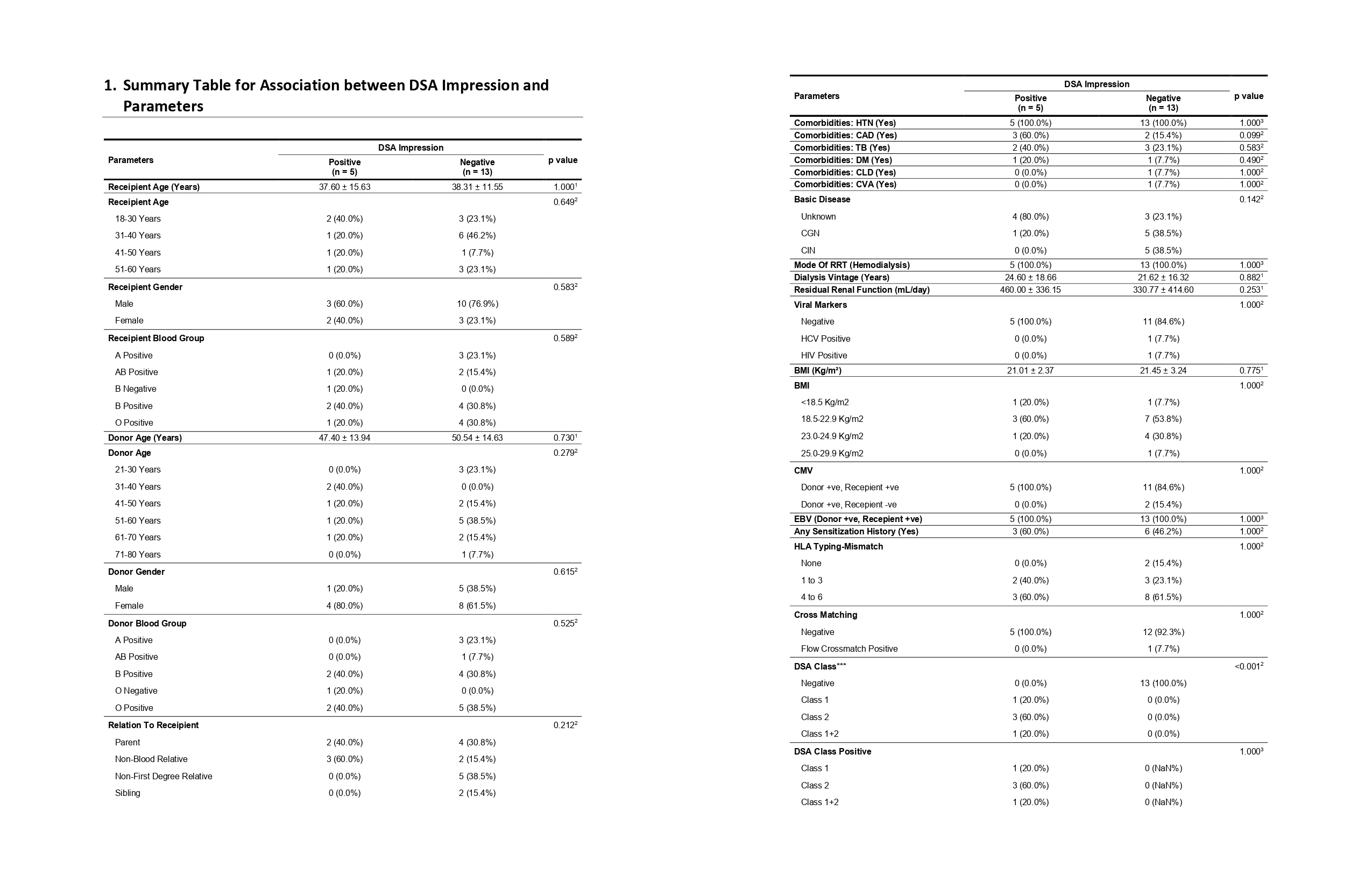
Materials and Methods: We retrospectively reviewed all adult kidney transplant recipients between January 2021 and March 2023.These patients were then divided by SAB reactivity into 2 groups in the setting of negative cross match.
1. Those with DSA
2. Those without DSA
Low dose desensitisation was done with plasmapheresis and IVIG prior to transplantation. Rejection, graft and patient survival were the outcomes measured.
Results: Of 18 patients, 5 were females and 13 males with mean age of 38 years. 13 (72.22%) patients had no DSA while 5 (27.77%) had DSA. Most commonly encountered DSA were against class 2 HLA primarily DQB1. Serum creatinine, eGFR were not significantly different between the 2 groups. At one year after transplantation, mean serum creatinine was 1.60 +/- 0.91 in DSA positive and 2.23 +/- 2.47 in DSA negative patients (p=0.84). The respective numbers for eGFR were 67.68 +/- 37.7 and 65.22 +/- 38.59 ml/min (p=1.0), and proteinuria (>500 mg/day) was seen in 20% and 15.4% (p=1.0) patients respectively. DSA positive patients had graft and patient survival rates that were not significantly different from those of DSA negative patients.
The incidence of rejection episodes was more frequent in DSA positive than in DSA negative patients (80%v/s 30.8%) without reaching statistical significance (p=0.118). None of them had hyper acute rejection.
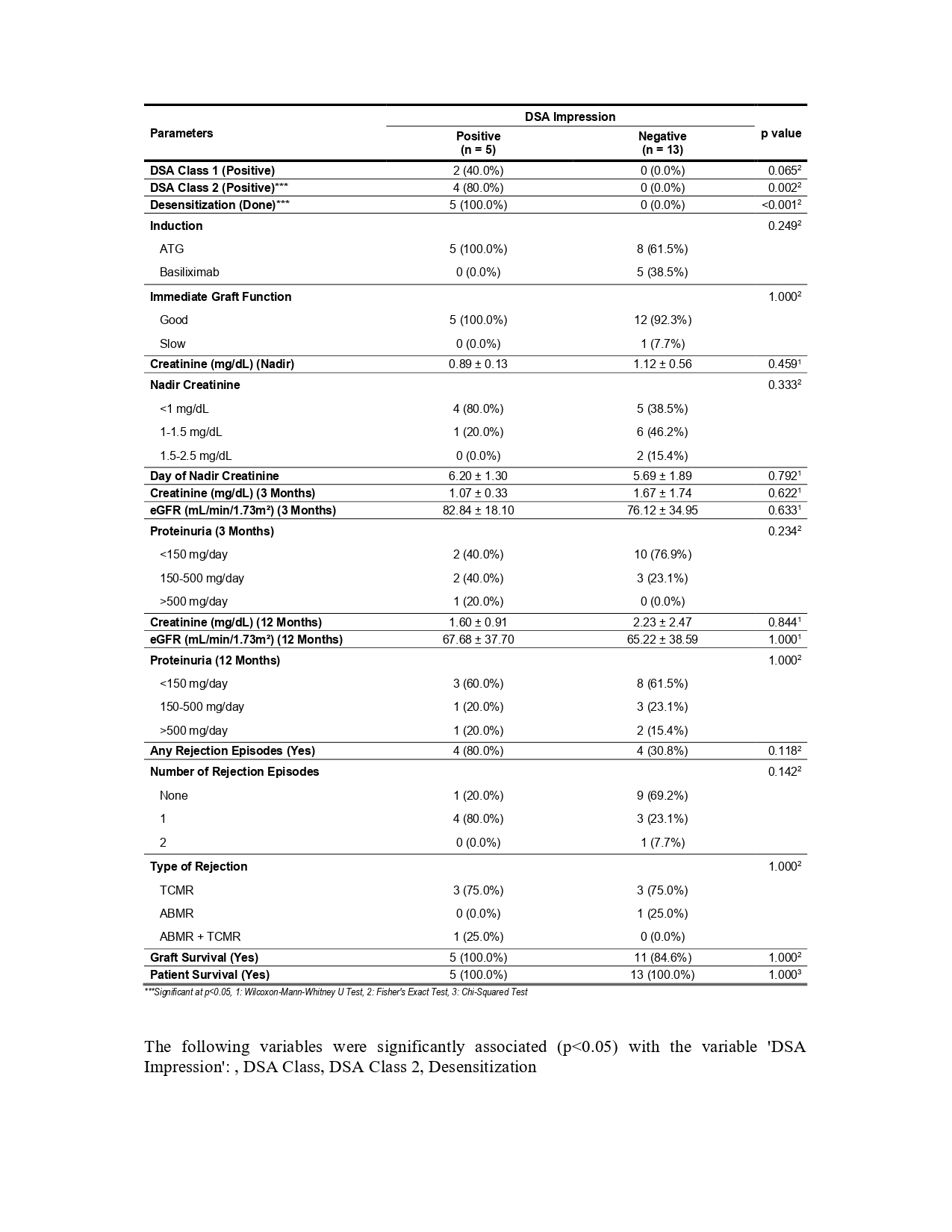
Discussion: To our best knowledge, there are very few reports on the subject of SAB DSA significance in living kidney recipients. In the context of increasing organ shortage, living donor kidney transplantation has not only become the optimal method of treating the end stage kidney disease but also an opportunity to expand the pool of potential donors. We observed excellent graft survival, a stable function of most of the transplant kidneys and low incidence of biopsy proven acute rejection episodes over one year period.
Conclusion: Our one year follow up of patients with pre transplant DSA treated with low dose desensitisation had graft and patient survival similar to patients with no DSA.
Study limitations- a larger cohort with pre transplant DSA was not available.
[1] Pre transplant donor- specific anti HLA antibody
[2] Kidney transplantation
[3] Low dose desensitisation
[4] Graft survival
[5] Patient survival
[6] Graft rejection
