
A prospective comparative study assessing learning curve of trainee surgeons in total laparoscopic versus hand assisted laparoscopic donor nephrectomy
Nasika Venkata Kanaka Naga Karthik1, Ashish Sharma1, Deepesh B Kenwar1, Sarbpreet Singh1, Kamal Kajal3, Jasmine Sethi2, Vivek Thakur1, Mohan Banoth1, Vanjinathan Subramani1, Amit Sharma1, Bharat Bhushan1, Sai Praneeth Reddy1, Sanjeev Chauhan1, Abhilash Tirkey1, Belmin B J Winston1.
1Renal Transplant Surgery, PGIMER, Chandigarh, India; 2Nephrology, PGIMER, Chandigarh, India; 3Anaesthesia, PGIMER, Chandigarh, India
Introduction: There are many studies comparing outcomes of total laparoscopic (TLDN) versus hand-assisted donor nephrectomy (HADN) but no prospective study has assessed the learning curve of trainee surgeons (TS) while initiating donor nephrectomy. The present study compared operative times, completion rates and outcomes of different individual steps of HADN vs. TLDN among different trainee surgeons.
Method: Four TS were assigned into two groups (HADN or TLDN) during the study period from February to December 2023. A total of 223 donor nephrectomies were done during this period. Each TS had similar prior laparoscopic and surgical experience. TS were allowed to be the primary surgeon only after having assisted at least 30 HADN or TLDN. Data about the first 15 cases operated by each TS under the supervision of a senior transplant surgeon (STS) was recorded. The procedure was divided into five phases with predefined time limits for each, after which the STS took over.
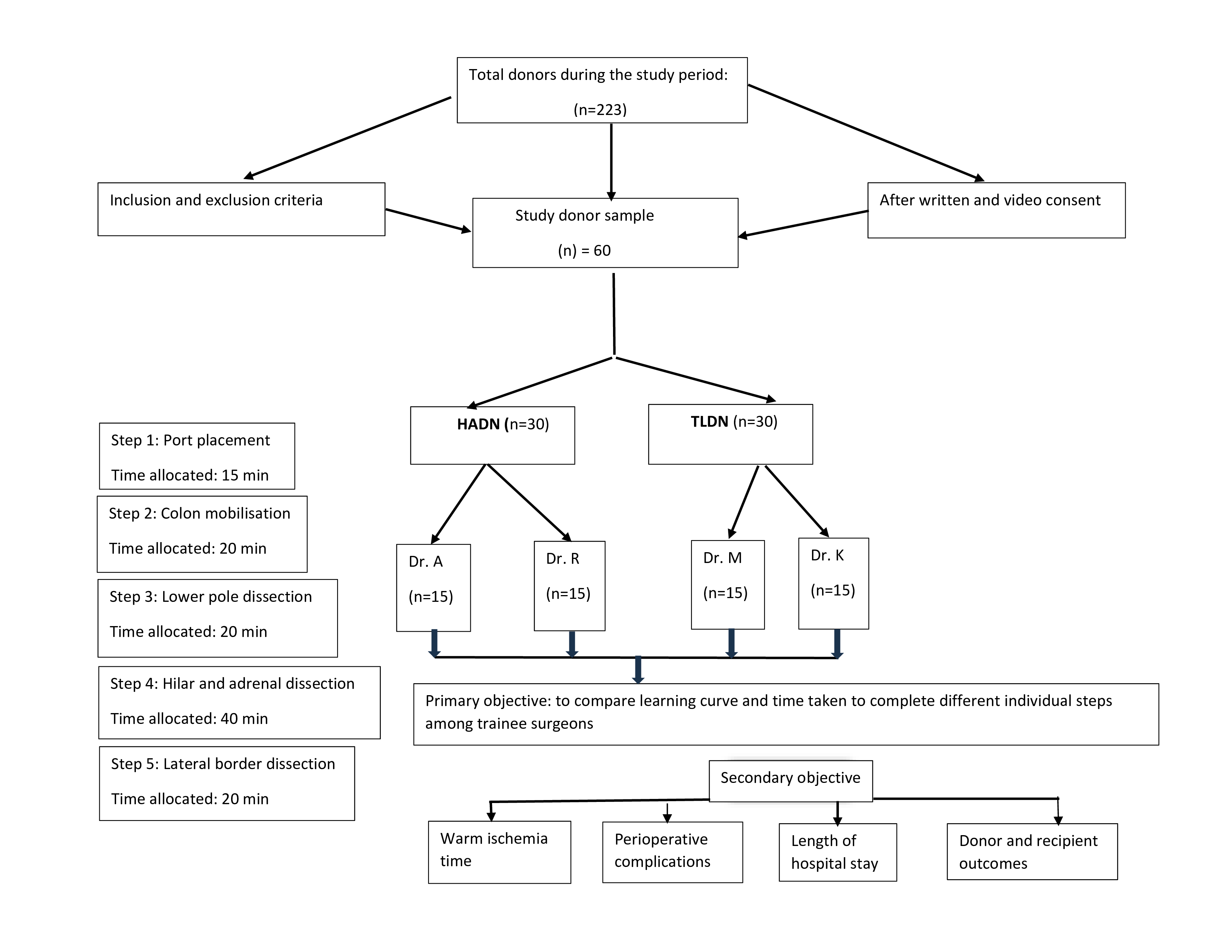
Demographic data, operative times for each phase of surgery, percentage completion of each phase, and need as well as indication for intervention by STS were recorded. The performance of the last 5 cases was compared with the first 5 cases of each TS.
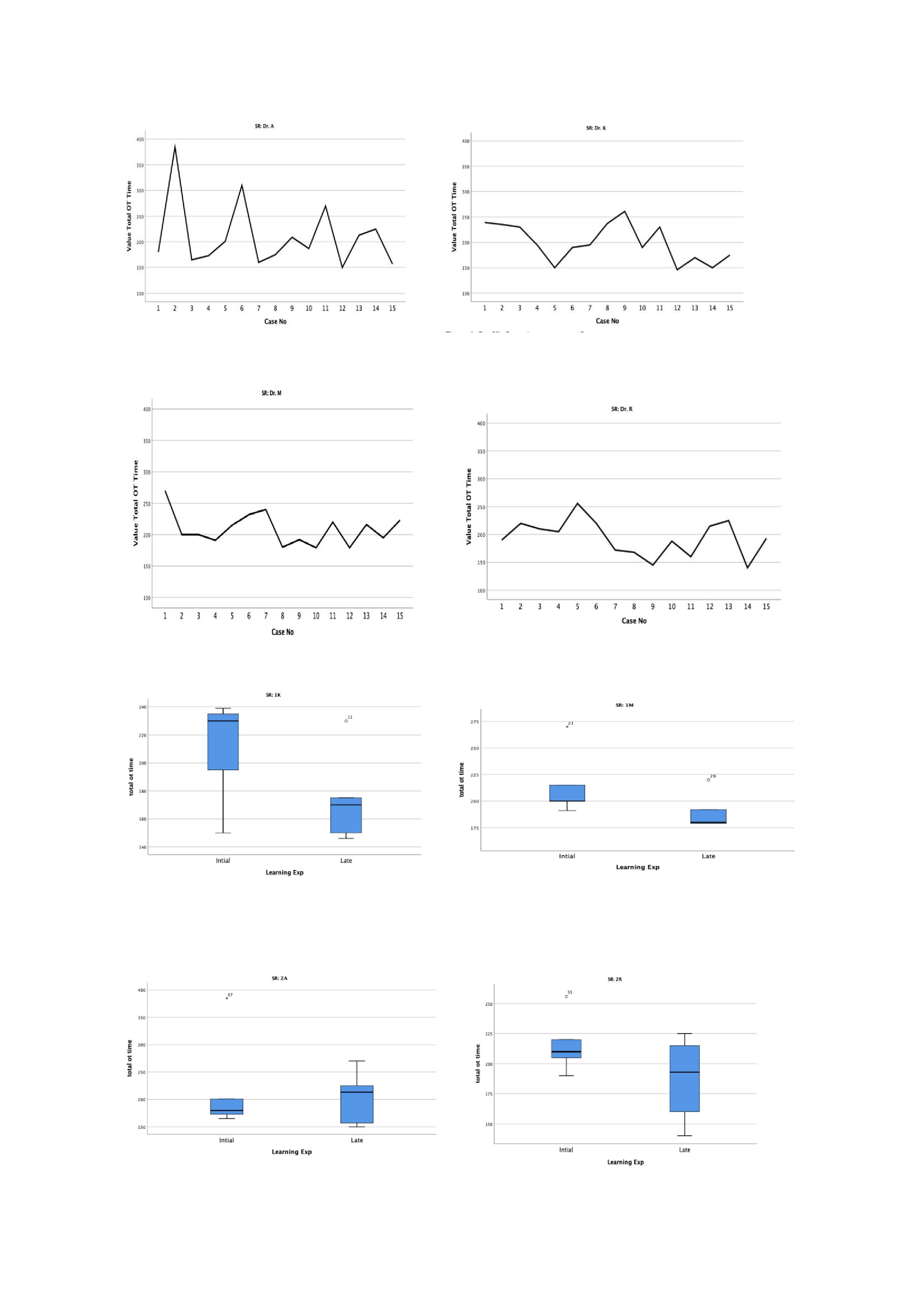
Mann Whitney test and median (25th and 75th percentile), maximum and minimum times were used to analyse phase-wise times. CUSUM plot was used to assess each TS’s learning curve. Statistical significance was kept at P<0.05.
Results: There was no difference in the total operative times between HADN vs. TLDN (197.5 vs.191 min; P = 0.26). Operative times decreased over the course of the study for all TS with wide variability although no tipping point was found. Colon mobilisation time (21.5 vs. 20 min; P = 0.02), hilum and adrenal dissection time (46.5 vs. 35 min; P =0.03) were lesser in HADN group. Lower pole dissection time was shorter in TLDN group (15 vs. 20 min; P = 0.009). Warm ischemia time was shorter in HADN than TLDN group (4 vs. 3min; P = 0.01), but donor and recipient outcomes were similar. STS intervention was required more often in the TLDN group (n=23 vs. n=7; P = 0.001). There were no conversions to open procedure. In two cases of TLDN, there was injury to unreported upper polar artery requiring bench reconstruction with no effect on donor and recipient outcomes. Postoperative complications did not differ between both the groups (P>0.05). No difference in operative time was noted with respect to age, gender, BMI, renal artery number, length of hospital stay, donor and recipient outcomes between both the groups (P>0.05).
Conclusion: Overall learning curve was shorter in HADN when compared to TLDN among TS. The donor and recipient outcomes as well as complications did not differ between the groups indicating safety when training surgeons with appropriate supervision under a structured academic programme with either technique.
OT supporting staff.
[1] Learning curve
[2] Total laparoscopic donor nephrectomy
[3] Hand assisted donor nephrectomy
[4] Trainee surgeon
[5] Time bound phases
[6] Warm ischemia time
[7] Perioperative complications
