A comparative analysis of kidney transplantation outcomes in systemic lupus erythematosus patients with disease flare vs. non-flare groups
Jin-Myung KIM1, Young-Eun Kim2, Hye Eun Kwon1, Youngmin Ko1, Joo Hee Jung1, Hyunwook Kwon1, Young Hoon Kim1, Seok-chan Hong2, Sung Shin1.
1Department of Surgery, Asan Medical Center, Seoul, Korea; 2Department of Internal Medicine, Asan Medical Center, Seoul, Korea
Introduction: Recently, kidney transplantation (KT) has emerged as a promising treatment for ESRD in LN patients, significantly reducing mortality rates. However, KT in LN patients carries the risk of post-transplant complications, including rejection, infections, and lupus disease flare. This study aimed to assess the incidence and clinical manifestations of lupus flare, particularly recurrent lupus nephritis, in kidney transplant recipients with a history of LN. Additionally, the study sought to identify potential risk factors associated with the occurrence of flare in this specific population.
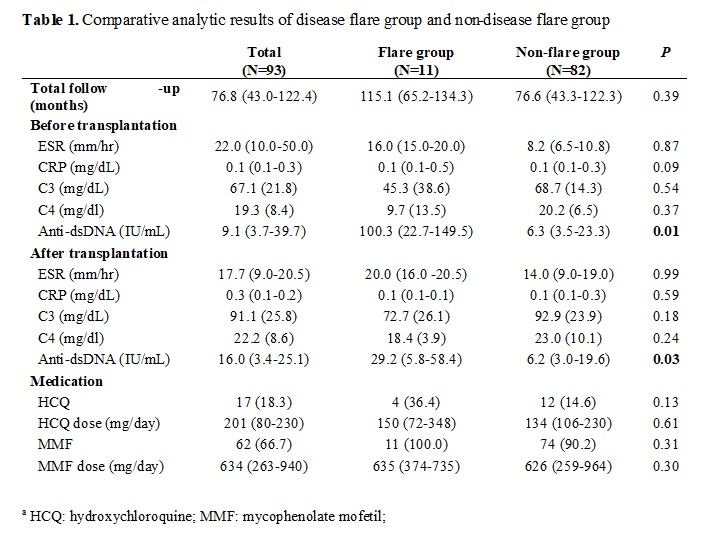
Method: A retrospective analysis was performed on 93 SLE patients who received kidney transplants at Asan Medical Center from January 1995 to December 2021. The patients were divided into two groups: the flare group, which experienced disease flares after transplantation, and the non-flare group, which remained in remission. The study collected and analyzed clinical data, including patient demographics, flare characteristics, immunosuppression regimens, patient survival, death-censored graft survival (DCGS) and biopsy-proven acute rejection (BPAR)-free survival rate.
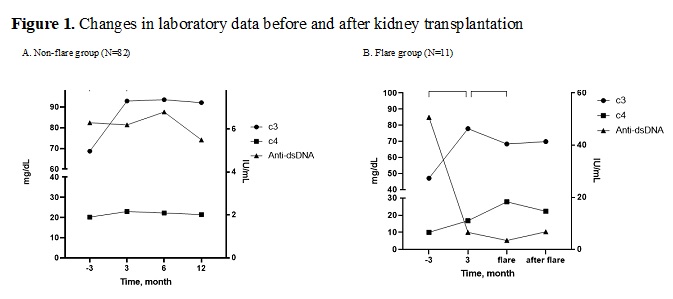
Results: Upon comparing flare (N=11) and non-flare (N=82) groups, the analysis found that patients who experienced a flare demonstrated elevated levels of anti-dsDNA prior to (100.3 vs. 6.3 IU/mL) and following (29.2 vs. 6.2 IU/mL) the kidney transplantation process. Notably, the anti-dsDNA level significantly decreased after transplant surgery for both groups. No significant changes were observed in other markers (ESR, CRP, and complement levels) or medication usage between the groups. During the disease flare, which occurred at a median of 8.0 months after transplantation, the most common manifestations were the recurrence of biopsy-proven lupus nephritis in 36.3% (4/11) of patients and hematologic manifestations in 36.3% (4/11) of patients. The median anti-dsDNA value during the flare was 3.5 IU/mL and eGFR was 26.0. The anti-dsDNA level before kidney transplantation was a predictive factor for flare (HR 1.030; 95% CI, 1.008–1.053; P = 0.008). The estimated 20-year patient survival was 83.3% for the flare group and 94.7% for the non-flare group, respectively (P=0.577). There was no significant difference in the DCGS rate between the two groups (P=0.435).
Conclusion: Our results suggest that anti-dsDNA level is a predictive factor for occurrence of flare in SLE patients who underwent kidney transplantation. The flare tends to occur within the first year after the transplantation and can lead to biopsy-proven lupus nephritis recurrence. In addition, regardless of the occurrence of flares, there is no significant difference in patient and graft survival rates. Further investigations are needed to identify optimal strategies for managing disease flares in SLE patients following kidney transplantation and to determine their impact on overall patient outcomes.
[1] Lupus
[2] recurrent disease
