
Dr. Koçak graduated from Hacettepe University School of Medicine in 1996. He completed his residency training in Urology at Türkiye Yüksek İhtisas Hospital in 2001. He finished his transplant surgery fellowship at Northwestern University Feinberg School of Medicine in 2004. He was a faculty member and the Director of the Kidney Transplant Program at Ondokuzmayıs University School of Medicine between 2005 and 2007. He served as the Director of The Kidney and Pancreas Transplant Programs at Memorial Şişli Hospital for over a decade (2007-2018). He was promoted to associate professor in 2011 and became a full professor in 2018. He joined Koç University Hospital as the Director of the Kidney and Pancreas Transplant Programs and a faculty member in 2018. Dr. Koçak is certified by The American Society of Transplant Surgeons for Kidney and Pancreas Transplantation.
Is native nephrectomy almost a must in low-weight pediatric kidney transplant patients?
Basak Akyollu1, Cemile Pehlivanoglu2, Cihan Karatas1, Emre Arpali3, Ilmay Bilge2, Burak Kocak1.
1Organ Transplantation, Koc University Hospital, Istanbul, Turkey; 2Pediatric Nephrology, Koc University Hospital, Istanbul, Turkey; 3Organ Transplantation, Medical College of Wisconsin, Milwaukee, WI, United States
Introduction: There is no consensus about indications and optimal timing for native nephrectomy (NNx) in pediatric kidney transplant (KTx) patients.
Method: This is a single center retrospective study reviewing pediatric KTx patients in terms of indications, timing and complications of NNx.
Patient and graft survivals were calculated with Kaplan-Meier survival analysis.
Results: Between July 2008 and December 2023, 112 children underwent living-related KTx.
Median recipient age was 3 years (range 0,6-17,4 years) with median body weight of 21,2 kg (range 6,4-47 kg).
NNx was performed in 42 patients (37,5%) in total. We performed NNx in 34 (30,3%) recipients in our instution and body weight was <15 kg in 25 of the patients (73,5%).
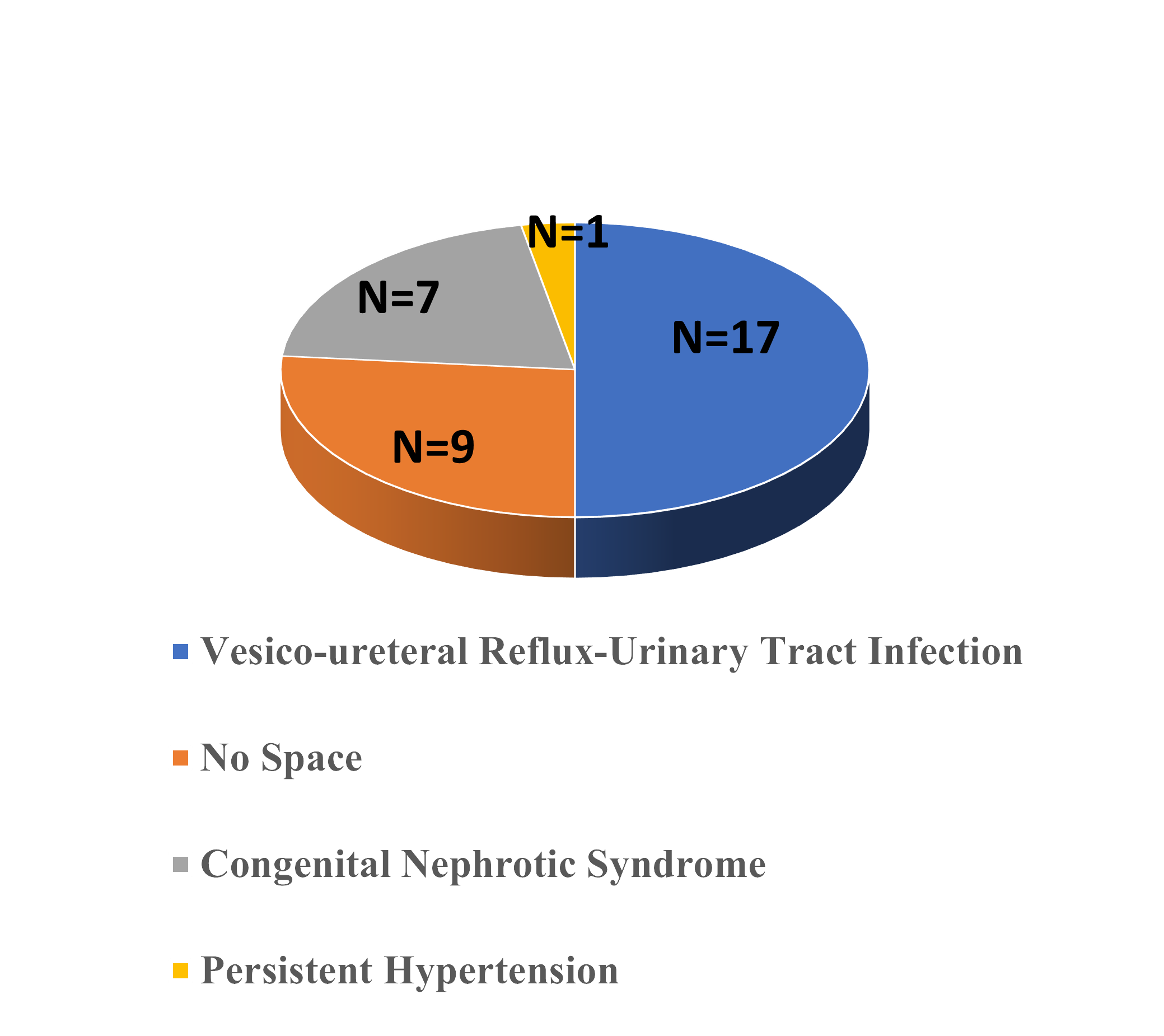
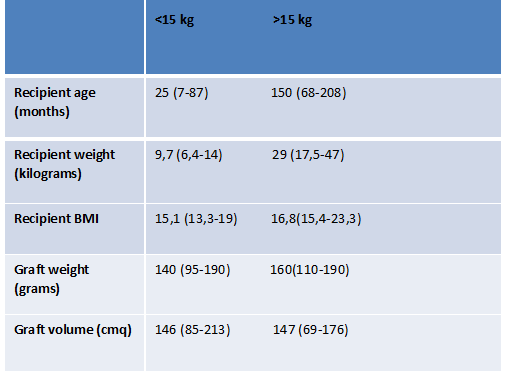
Only one 10-month-old, 6,4 kg patient with ARPKD had staged nephrectomy prior to KTx and the rest of the NNx were done simultaneously. 6 patients had a history of unilateral and 2 patients had a history of bilateral NNx performed in outer centers prior to their transplant. The median time interval to transplant following NNx was 24 months (range 3-132 months). 25 of the total 37 low weight pediatric KTx patients (68%) required NNx in the whole series.
Transabdominal approach was the choice in 28 patients including staged NNx case and the rest were performed by retroperitoneal approach with extended right sided hockey stick incision. All of the bilateral NNx (n=20) and all (n=2) left sided unilateral NNx were done by transabdominal approach. In 12 patients we performed right sided unilateral NNx by retroperitoneal approach with extended right sided hockey stick incision for the 6 patients and for the rest of the 6 patients transabdominal approach was the choice.
All patients with NNx are alive with well-functioning allografts at 19,2 months (range 0,6-62,6 months) of median follow up period.
Overall patient and graft survivals are 98,2% and 97,3% respectively at 20,6 months (range 0,4-66,5 months).
The post-operative surgical complications in patients who had NNx in our instution were intestinal obstruction (n=2) and one of these 2 patients had also developed urine leak (n=1) which required laparotomy during the follow up and the other one had a history of a previous intraabdominal surgery naming left surrenalectomy for a neuroblastoma 3 years before the KTx. The other complications were evisceration (n=1) and surgical site hemorrhage (n=1) which received red blood cell transfusion as the sole management for the bleeding. There was no arterial/venous thrombosis nor uretero-vesical stricture of implanted grafts.
One of our patient who had a history of bilateral NNx in outer center 2 years before KTx due to Wilms tumor, whose KTx was performed by retroperitoneal approach, developed ileus at post-operative day 5 which also required laparotomy.
Conclusion: NNx at the time of KTx is a safe procedure with manageable morbidities especially in low body weight children.
[1] transplantation
[2] kidney
[3] pediatric
[4] nephrectpmy
