
Dr. Koçak graduated from Hacettepe University School of Medicine in 1996. He completed his residency training in Urology at Türkiye Yüksek İhtisas Hospital in 2001. He finished his transplant surgery fellowship at Northwestern University Feinberg School of Medicine in 2004. He was a faculty member and the Director of the Kidney Transplant Program at Ondokuzmayıs University School of Medicine between 2005 and 2007. He served as the Director of The Kidney and Pancreas Transplant Programs at Memorial Şişli Hospital for over a decade (2007-2018). He was promoted to associate professor in 2011 and became a full professor in 2018. He joined Koç University Hospital as the Director of the Kidney and Pancreas Transplant Programs and a faculty member in 2018. Dr. Koçak is certified by The American Society of Transplant Surgeons for Kidney and Pancreas Transplantation.
Native nephrectomy in autosomal dominant polycystic kidney disease patients for kidney transplantation: Do we really need it?
Cihan Karataş1, Başak Akyollu1, Emre Arpalı1, Mehmet Kanbay1, Yakup Kordan1, Burak Kocak1.
1Organ Transplantation Center, Koç University Hospital, Istanbul, Turkey
Introduction: Although, native nephrectomy (NNx) is commonly performed in kidney transplant (KTx) recipients with ADPKD, the timing, indications, and surgical approach vary depending on the center's protocols or symptomatic presentations reported relatively by the patients. The necessity to create space for KTx is particularly a relative and arguable indication for a NNx. This study reviews the rationale, surgical methodologies, and outcomes in KTx patients with or without NNx in the context of ADPKD.
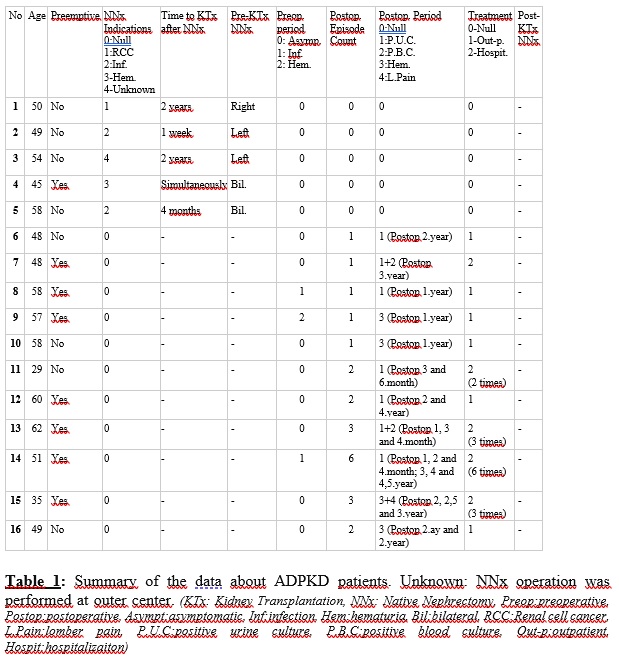
Method: We retrospectively evaluated adult patients with ADPKD who underwent KTx between 2018 and 2023 at our institution. Data regarding the timing and techniques of NNx, postoperative complications, patient and graft survivals were collected. Patients were assessed for a history of recurrent urinary tract and/or severe cyst infections, hematuria, complications secondary to the mass effect of the polycystic kidneys and other NNx indications before and after KTx. Preoperative and postoperative-if available- dimensions of the polycystic kidneys in the CT scan were reported.
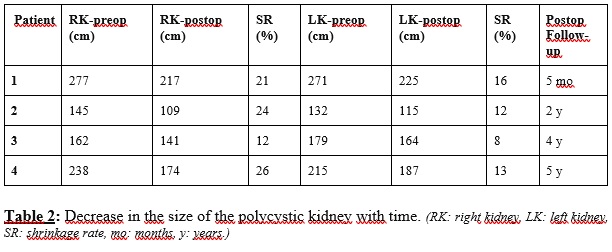
Results: Among 566 KTx performed, 39 were due to ADPKD. There were 21 female (48%) and 22 male (52%) patients, with an average age of 51.6±8.6years, and with an average BMI of 27.5±5.6. Preoperatively, 5 (12%) of the patients experienced frequent urinary tract and/or severe cyst infections, and 2 (5%) had hematuria episodes. 5 patients underwent NNx. 3 patients had unilateral and 2 had bilateral NNx. One patient had a simultaneous bilateral NNx with KTx due to recurrent hematuria and all the others underwent NNx prior to KTx at intervals ranging from 4 months to 2 years due to cyst infection, recurrent nephrolithiasis, and renal cell carcinoma. There was no indication of mass effect or to create space for KTx in the etiology of NNx (Table 1). The average length of the right and the left kidneys were 185±42cm and 183±40cm, respectively. During postoperative follow-up, CT scans performed in 4 patients for cause revealed a reduction in the size of the polycystic kidneys (Table 2). Postoperatively, the average hospital stay was 7.56±5.7days, with a median outpatient follow-up of 2 (range: 0.1-4.5)years. One patient died in the 4th postoperative year due to COVID pneumonia.
7 of the patients (17%) had complaints related to infection and 5 (13%) had complaints related to hematuria. While 4 (10%) of the patients complicated by infection required repeated hospitalization, only 1 (2%) of the hematuria patients required repeated hospitalization. None of the patients required NNx in the postoperative period.
Conclusion: NNx in KTx patients with ADPKD could be utilized for a very rare group of patients. NNx for anatomical space considerations for a KTx is never necessary and a successful KTx could be carried out despite how big the native kidneys are. NNx after KTx is rarely needed probably due to further potential decrease in the size of the polycystic kidneys reported by studies.
[1] ADPKD
[2] kidney transplantation
[3] polycystic kidneys
[4] native nephrectomy
