
Urinary tract infections in kidney transplant recipients: Antimicrobial treatment choices are decreasing
Nuran Sari1, Tuba Kurt1, Ozlem Kurt Azap1, Hande Arslan1, Emre Karakaya2, Mehmet A. Haberal2.
1Department of Infectious Diseases and Clinical Microbiology, Baskent University, Ankara, Turkey; 2Department of General Surgery, Division of Transplantation, Baskent University, Ankara, Turkey
Introduction: Urinary tract infections (UTIs) represent a prevalent complication among kidney transplant recipients, contributing significantly to both morbidity and mortality. The escalating resistance to antimicrobial agents, a phenomenon observed across various infectious contexts, poses substantial challenges in the effective management of UTIs. Understanding the local antimicrobial resistance landscape is imperative for guiding empirical treatment strategies at individual centers.
Method: A retrospective review of medical records spanning from January 2017 to December 2023 at Baskent University Ankara Hospital was conducted, focusing on kidney transplant recipients aged 18 and above. Key parameters assessed included the identification of common causative pathogens, antimicrobial resistance profiles against frequently used antibiotics (colistin, amikacin, ciprofloxacin, meropenem, trimethoprim/sulfamethoxazole), rates of extended-spectrum beta-lactamase (ESBL) positivity, and multidrug resistance. Demographic and laboratory data were analyzed using SPSS 25 statistical software, adhering to ethical principles.
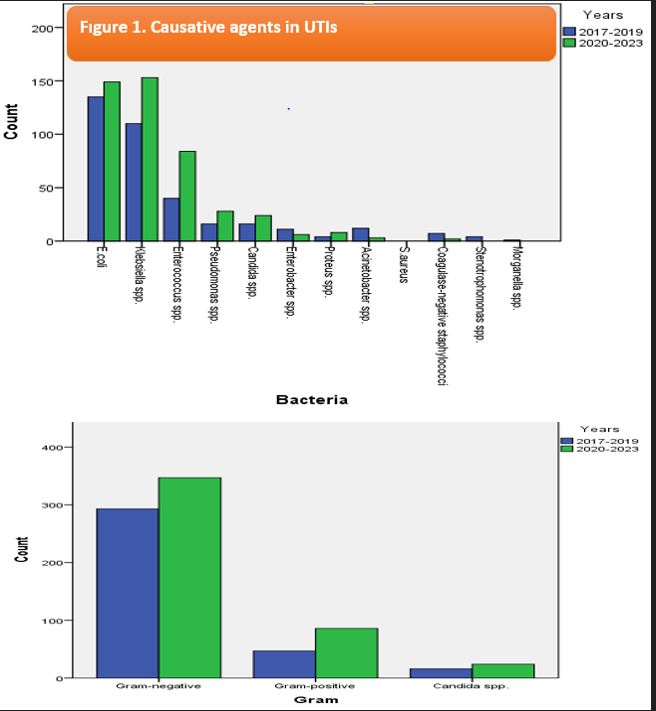
Results: During the seven-year study period (2017-2023), 441 kidney transplant recipients experienced a total of 813 UTIs episodes. Among these patients, 434 (53.3%) were female, with a median age of 46±14.5 years (range: 18 to 72). Causative pathogens included 540 (66.4%) gram-negative bacteria, 133 (16.3%) gram-positive bacteria, and 40 (4.9%) Candida spp. The mean value of blood cultures positivity was determined as 5.5%. The most frequently encountered infectious agents were Escherichia coli, Klebsiella pneumoniae, Enterococcus spp., Pseudomonas spp., and Candida spp. (Fıgure 1). ESBL positivity among E. coli and Klebsiella spp. ranged from 45% to 67%, while pundrug resistance prevalence varied from 1% to 16%, exhibiting an upward trend over the study period. Resistance rates to ciprofloxacin and trimethoprim/sulfamethoxazole exceeded 70%, whereas resistance to carbapenems, colistin and amikacin increased to around 30%, with increasing trends observed over time.
Conclusion: Enteric bacteria, particularly E. coli, K. pneumoniae, and Enterococcus spp., predominate in UTIs among kidney transplant recipients. Our findings highlight a concerning surge in resistance to ciprofloxacin and trimethoprim/sulfamethoxazole, potentially limiting their utility in empirical treatment and prophylaxis. Moreover, escalating rates of ESBL and multidrug resistance underscore the imperative of targeted treatment guided by urine culture results in symptomatic patients.
[1] Antimicrobial Resistance, Kidney Transplant, Urinary Tract Infections
