Is celulitis always cellulitis? Unusual manifestation of cryptococcosis in solid organ transplantation: A case report
Cigdem Erol1, Ozan Yildiz1, Tuba Kurt1, Bahtiyar Haberal2, Hande Arslan1, Mehmet A. Haberal3.
1Department of Infectious Diseases and Clinical Microbiology, Baskent University, Ankara, Turkey; 2Department of Orthopedics, Baskent University, Ankara, Turkey; 3Department of General Surgery, Division of Transplantation, Baskent University, Ankara, Turkey
Introduction: Cryptococcus is an environmental fungus exist in the soil, trees, and bird droppings and cryptococcosis is the third most common invasive fungal infection in SOT recipients. The mortality rates for all types of solid organ transplant patients with cryptococcosis vary from 14% to 19.6% and can reach up to 50% in recipients with meningitis.
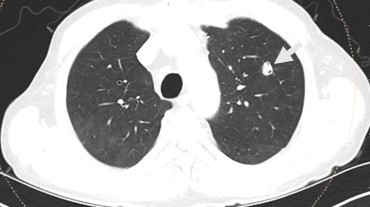
Case: A 65-year-old male patient with a history of kidney transplantation 10 years ago was admitted to outpatient clinic for erythema and edema on the dorsum of his left foot. He had no history of trauma. He was diagnosed with cellulitis due to leukocytosis and elevated CRP levels with his symptoms, and subsequently got oral antibiotic therapy. One week after the redness subsided, the discomfort intensified and CRP levels elevated further. Foot MRI has been performed and osteomyelitis in his fifth mettarsal bone has been investigated (figure 1). An MRI of the foot was conducted to evaluate osteomyelitis in the fifth metatarsal bone. Following a further 6 weeks of intravenous antibiotic treatment, a fistula developed, leading to a debridement surgery for sampling. Cryptococcus neoformans serotype A was isolated from bone tissue culture and treatment with fluconazole was initiated. A nodular lesion was observed in his chest CT scan despite the lack of respiratory symptoms (figure 2). There were no neurological symptoms or meningeal involvement observed in the cranial MRI, nevertheless, a lumbar puncture was conducted. A positive Cryptococcus neoformans latex agglutination test was detected in the cerebrospinal fluid analysis, requiring a change in his antifungal treatment to liposomal amphotericin B for disseminated disease involving central nervous system. During the same week, prostate imaging was conducted due to urinary retention, and an abscess was examined. Cryptococcus neoformans serotype A was cultured from the abscess after it was drained. Following a 4-week course of Liposomal amphotericin B treatment, antifungal medication was changed to fluconazole and continued for 12 months until full recovery and no complications or immune reconstitution inflammatory syndrome (IRIS) occurred, although a urinary tract infection developed during the therapy.
Conclusion: Cryptococcosis should be considered in the differential diagnosis of cellulitis and osteomyelitis in renal transplant recipients. To effectively manage this infection, it is essential to utilize all microbiological and molecular techniques available due to its severity and invasive nature. Early identification plays a critical role in determining the prognosis of this illness.