Biliary sludge and complications in multivisceral transplantation patients
Carmelo Loinaz1,2,3, Jorge Calvo1,2,3, Felix Cambra1,2,3, Alejandro Manrique1,2,3, Alvaro Garcia-Sesma1,2,3, Iago Justo1,2,3, Oscar Caso1,2,3, Alberto Marcacuzco1,2,3, Clara Fernandez1,2,3, Andres Del Pozo3,4, Jose Diaz Tasende3,4.
1Surgery, Hospital Universitario 12 De Octubre, Madrid, Spain; 2Surgery, Complutense University Of Madrid, Madrid, Spain; 3Research Institute, Hospital Universitario 12 De Octubre, Madrid, Spain; 4Gastroenterology & Hepatology, Hospital Universitario 12 De Octubre, Madrid, Spain
Introduction: Though biliary complications are frequent in the field of liver transplantation, the descriptions of complications related to biliary sludge are scarce in multivisceral transplantation (MVT). We present here 3 cases of biliary sludge and related complications in recent years.
Description of cases:
Case 1: a 50 y old woman with a MVTdone 5 months before for SBS due to SMA thrombosis and PNALD, and simultaneous kidney transplant with a 99% PRA, was diagnosed of invasive aspergillosis. During her last days, a biliary cast was observed at CT scan, and biliary necrosis and perforation, with Candida, was observed at necropsy.
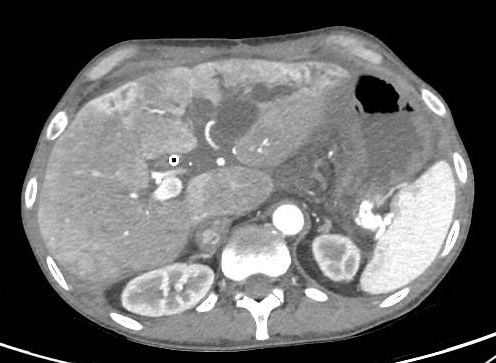
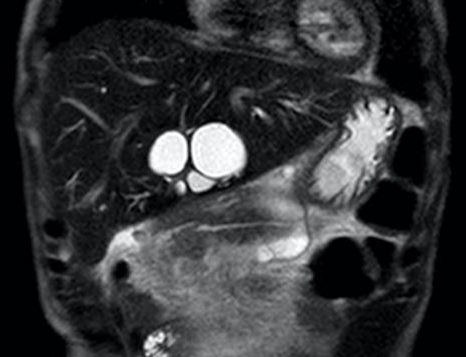
Case 2: a 52 y old man, with a MVT for diffuse portomesenteric thrombosis, Budd-Chiari syndrome and a thrombosed portocaval shunt. He showed cholestasis since 2 weeks of the procedure, initially related to drug toxicity, but progressively deteriorated, and biliary sludge was shown after several weeks, an ERCP failed, a PTC was done and a bile cast shown. Repeated ERCPs were done for cholangitis and stent exchange, and he developed intrahepatic massive biliary dilation (see figures 1 and 2). Over time, antibiotic resistant bacteria were isolated. A left liver lobe resection and bilioenteric anastomosis were done with the aim to stop these complications, but a severe sepsis developed and the patient subsequently died, 2 1/2 years after the MVT.
Case 3: a 45 y old man, with a MVT for Gardner´s syndrome with a big duodenal adenoma with severe dysplasia and short bowel syndrome. He showed progressive cholestasis after 6 weeks, starting with ursodeoxycholic acid, and biliary sludge after 10 weeks. He had an ERCP with biliary sludge and microlithiasis removal. A stent was avoided. A second ERCP was done 18 weeks after MVT, without stenting. The patient is now (5 1/2 months after MVT) without symptoms and normal LFTs.
Discussion: It is difficult to know the cause of biliary sludge in these cases, most probably multifactorial: denervation with dysfunction of the sphyncter of Oddi, fasting, parenteral nutrition, bile duct ischemia, etc. Sludge is common after bone marrow transplantation, and cardiac and kidney transplants, though it resolves in many cases. Case 1 appeared as a preterminal complication and it is difficult to ascertain if the reason was the fungal infection itself. Case 2 developed a predominant saccular dilation of the left biliary tree, with repeated severe cholangitis. We opted for the surgical treatment, but with a fatal outcome. Case 3 needs a longer follow-up to see the result.
Conclusion: Biliary sludge and microlithiasis after MVT is probably more a common complication than expected or reported
Currently, its origin is not clear, and the optimal treatment has to be ellucidated
To the Intestinal Failure and Rehabilitation Unit of the 12 de Octubre Hospital.
[1] multivisceral transplantation
[2] biliary sludge
