
Psychosocial factors and immune tolerance in liver transplant recipients: insights from a cohort study
Nasrin Motazedian1, Alireza Shamsaeefar2, Seyed Ali Moosavi1, Sanam Faizabadi1, Amirali Mashhadiagha1, Hamed Nikoupour2, Arvin Hedayati3, Siavash Gholami2, Ali Nowroozi1, Saman Nikeghbalian2.
1Transplant Research Center, Shiraz University of Medical Sciences, Shiraz, Iran; 2Abu Ali Sina Organ Transplant Center, Shiraz University of Medical Sciences, Shiraz, Iran; 3Department of Psychiatry, Shiraz University of Medical Sciences, Shiraz, Iran
Introduction: Liver transplantation is pivotal for end-stage liver disease, but lifelong immunosuppressants pose risks. Inducing tolerance offers a solution, especially in the liver due to its unique capabilities. Depression and anxiety, impact post-transplant outcomes. However, their association with immune tolerance remains underexplored. This study aims to assess the relationship between depression, anxiety, and immune tolerance post-liver transplantation.
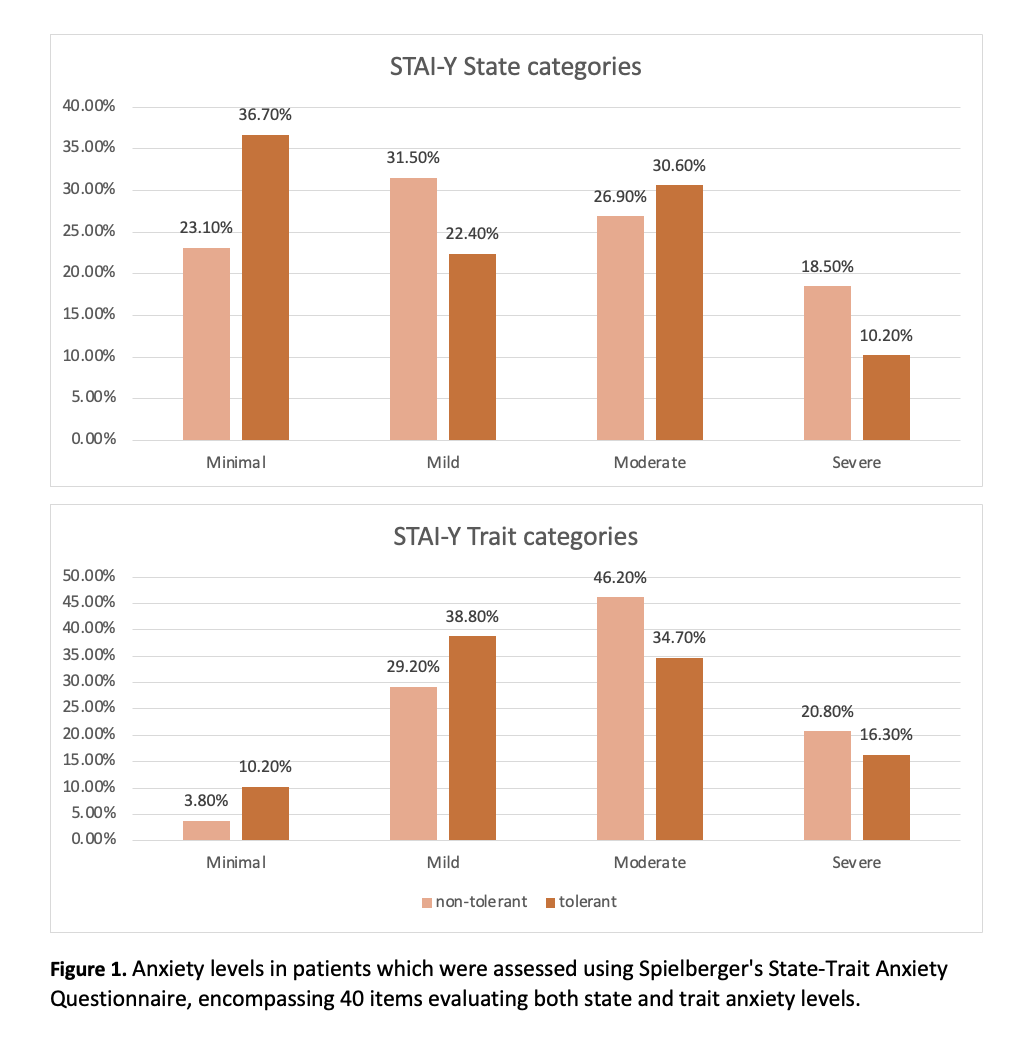
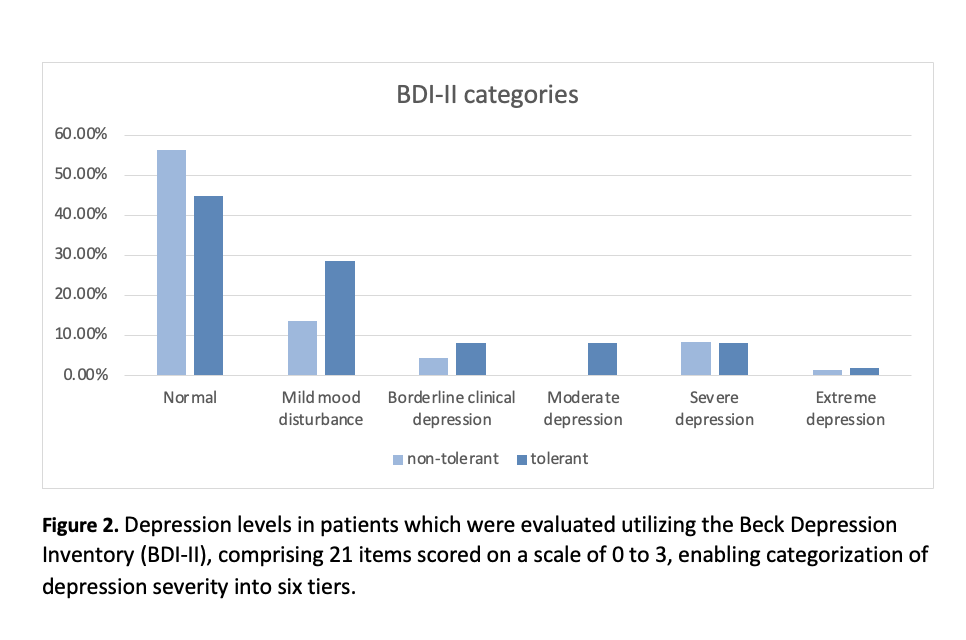
Method: This cohort study enrolled liver transplant recipients aged 18 to 45 who underwent liver transplantation and had been on immunosuppressive therapy for at least 6 months. Patient selection involved reviewing the medical records of 3,843 LT recipients, selecting individuals with optimal liver function parameters. Finally we included 179 LT patients, with 130 in the control group receiving standard immunosuppressive (IS) regimen and 49 in the case group receiving monotherapy with IS regimen, defined as prope tolerant. Exclusion criteria encompassed refusal to participate, recent hospitalization, antidepressant or antianxiety medication use pre- or post-transplant, or a history of transplant rejection. Depression levels were assessed using the Beck Depression Inventory (BDI-II), while anxiety levels were evaluated with Spielberger's State-Trait Anxiety Questionnaire (STAI-Y). The analysis of the obtained information was done using descriptive statistical methods and statistical tests of correlation coefficient and t-test and chi-square at the 5% significance level.
Results: The cohort study included 179 liver transplant recipients, predominantly male (64.2%), with a mean age of 39.36 ± 14.01 years and a majority married (83.2%). A history of psychiatric disorders, i.e., depression and anxiety disorders, was observed in 19.0% and 53.1% of patients, respectively. Common comorbidities were ulcerative colitis (9.5%), type two diabetes (8.9%), and cardiovascular diseases (3.9%). Around 27.4% exhibited immune tolerance. Marital status significantly predicted immune tolerance, with married patients showing higher odds. Ulcerative colitis was more common among non-tolerant patients, while anxiety disorders were less prevalent in tolerant patients. Based on the scores obtained from the Beck questionnaire, there was no significant difference between the depression scores of the non-tolerant group (12.45 ± 11.38) and the tolerance group (13.14 ± 10.67). Also, for STAI-Y State and Trait total scores, there were no significant differences between non-tolerant and tolerant groups (p = 0.085 and p = 0.102, respectively).
Conclusion: This suggests that depression and anxiety are prevalent among liver transplant patients, but they may not be directly linked to the development of immune tolerance. While our study provides valuable insights into the complex interplay between psychosocial factors and immune tolerance in liver transplant recipients, further research is warranted.
[1] End-stage Liver Disease, Liver Transplant, Tolerance, Depression, Anxiety
