A step towards bridging the gender gap in deceased donor kidney transplantation
Khushboo Saxena1, Vivek Kute1, Himanshu Patel1, Divyesh Engineer1, Subho Banerjee1, Jamal Rizvi2, Pranjal Modi2.
1Department of Nephrology, Institute of Kidney Disease and Research Centre-Institute of Transplantation Sciences, Ahmedabad, India; 2Department of Urology, Institute of Kidney Disease and Research Centre-Institute of Transplantation Sciences, Ahmedabad, India
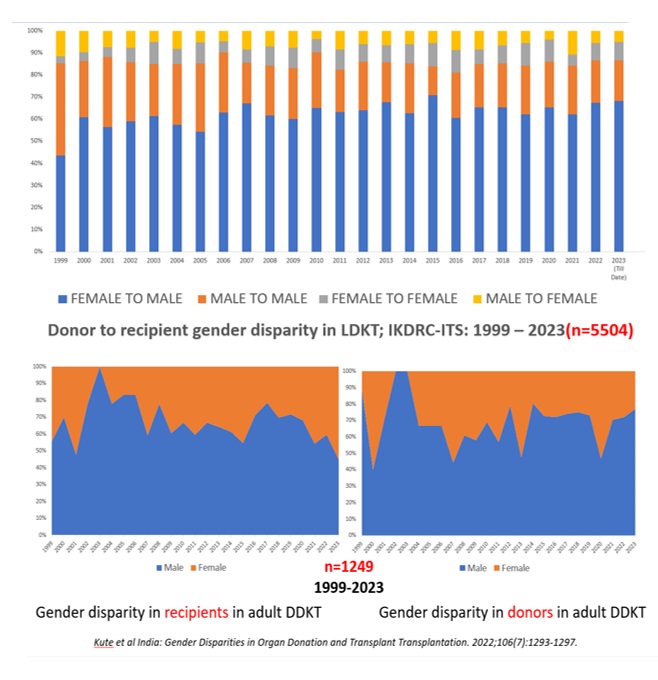
Introduction: Overcoming gender disparity in access to kidney transplantation is a well-established universal challenge. The SRTR data showed a greater proportion of males than females for kidney transplant waitlists (61% vs 39%). Similarly, of 831 deceased donor kidney transplants (DDKT) conducted between 1997 and 2018 at IKDRC-ITS, 68% have been male and 32% female recipients while majority of donors in living donor kidney transplants (LDKT) were females.
Prior to 2020, duration on transplantation waitlist was the only criteria for deceased donor kidney allocation. In January 2020, SOTTO Gujarat was formed which implements a point system based deceased donor allocation policy including HLA mismatch, Panel Reactive Antibody, Donor Specific Antibody, age and duration on dialysis, amongst others. 2 additional points are allocated to female recipients in this allocation system. The aim is to study the impact of change in DDKT allocation policy on gender disparity.
Methods: This is a retrospective, single-center, observational study. Number of male and female kidney transplant recipients was collected from the medical records held by the department of nephrology between January 2014 to December 2023. The data was categorized as before and after implementation of SOTTO Gujarat guidelines and analyzed.
Results: A total of 3182 kidney transplants were conducted at our centre over the study period, 2231 were LDKT while only 951 were DDKT. Out of 393 kidney paired donations conducted over the study period, 79.64% recipients were males. We found the percentage of female LDKT recipients to have remained disproportionately low as compared to male DDKT throughout the study period, while there was a gradually progressive increase in the percentage of female DDKT recipients with almost a doubling of female DDKT recipients from 27.57% in 2019 to 54.19% in 2023. This may be attributed to the compounding effect of allocating points to DSA, PRA, age of patient and gender as female patients tend to have higher PRA and DSA level after sensitization.
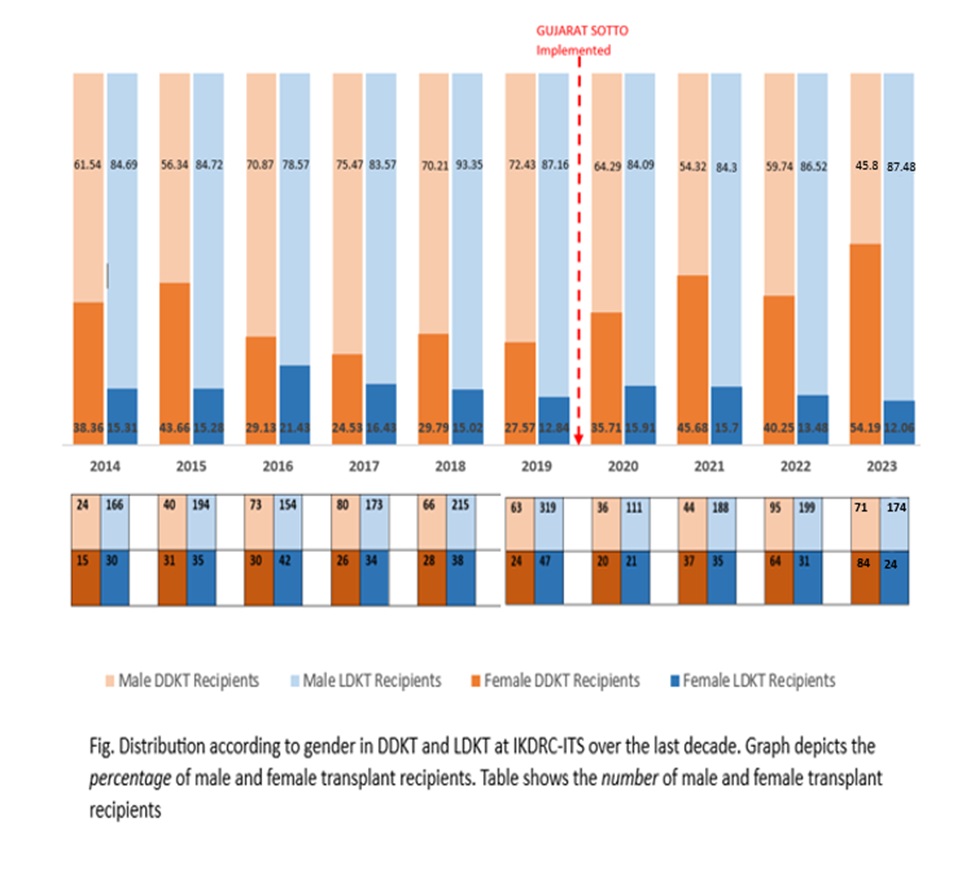
Conclusion: This study provides new insights into steps that can be taken to bridge the gender gap in DDKT. Implementing a point based system for DDKT allocation policy with extra points for female recipients may increase the number of kidney transplants in them. Similar policy may be undertaken by other centers as a bridge to achieve temporary solution till underlying factors leading to gender disparity are better understood and ways to overcome them are formed. Action should be taken to provide for equitable access to females at all stages, from diagnosis to treatment. Policies for social empowerment of women must be formed including literacy, better maternal and child healthcare and financial independence. Raising awareness and education at a grassroot level is key component to change public attitude regarding organ donation and ensure equitable access to transplantation.
