Kidney transplantation in the biggest Croatian abdominal organs transplantation center during COVID-19 pandemics (11 March 2020 – 11 May 2023)
Ksenija Vučur Šimić1, Željka Jureković1, Lada Zibar1,2.
1Department of Nephrology, Internal Clinic, University hospital Merkur, Zagreb, Croatia; 2Department for Pathophysiology, Faculty of Medicine, University Josip Juraj Strossmayer , Osijek, Croatia
Introduction: Recent COVID-19 pandemics presented a jeopardy to all health spheres including transplantation (TX) access. University Hospital Merkur in Zagreb, Croatia, continued its kidney TX within Eurotransplant during that more than three years time almost without interruption. All epidemiologic measures were respected and we avoided lymphocyte depleting therapy.
Aim: To present the course and results of kidney TX at our center during pandemics.
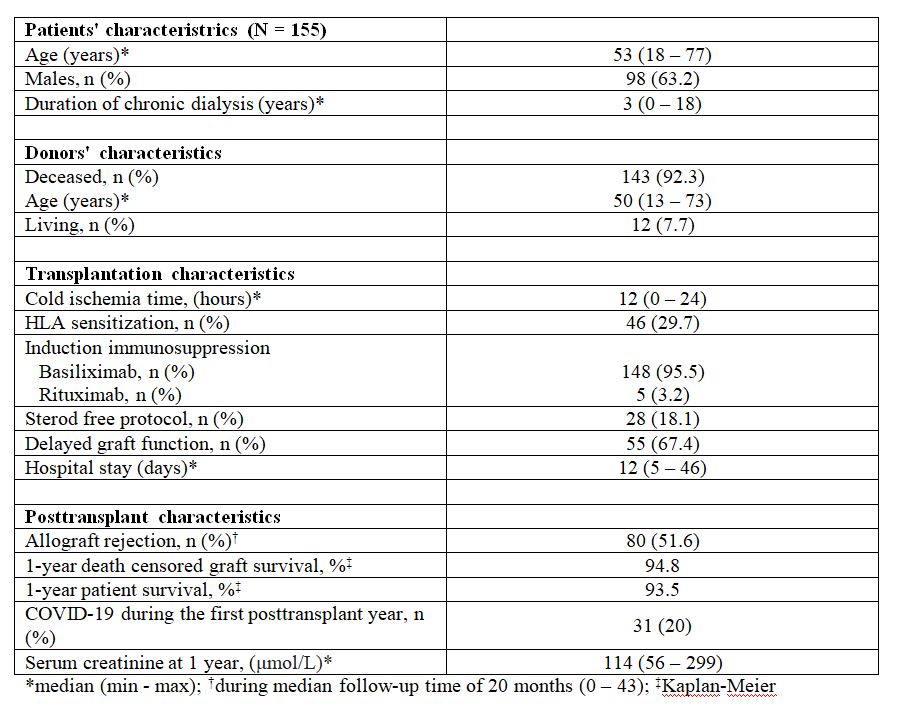
Methods: The data on patients, donors, TX and follow-up (FU) features were taken from medical records. We covered the 38 months’ period 11 March 2020 – 11 May 2023, the official pandemics time in Croatia. We also recorded the number of kidney TXs during the 38 months’ period just preceding the pandemics. Kaplan-Meier survival analysis was used.
Results: A total of 155 patients (98 males, 63.2 %; median age 53 years, 18 – 77; median dialysis duration 3 years, 0 – 18; 13 preemptive, 8.4 %) kidney TXs were performed, thereof 16 combined with pancreas TX and 6 with liver TX. 22 TXs were in 2020, after the 11 March, 51 in 2021, 49 in 2022 and 33 in 2023, until the 11 May. In 12 patients it was the second (7.7 %) and in 4 the third kidney TX (2.6 %). The organs were from deceased donors in 143 cases (92.3 %, median age 50 years, 13 - 73), while 12 were living donations (7.7 %). Median cold ischemia time was 12 h (0 – 24). One third of patients were sensitized to HLA antigens (median vPRA 62.32 %, 0.85 - 99.2). Induction therapy with basiliximab was applied in 148 (95.5 %) and rituximab in 5 patients (3.2 %). Median hospital sojourn was 12 days (5 – 46). Maintenance immunosuppression consisted of standard therapy with tacrolimus and mycophenolate with or without steroids (28 steroid free patients, 18.1 %). Delayed graft function ensued in 55 (35.5 %) patients. Hospitalization during the first postTX year was recorded in 83 patients (67.4 %). During the median FU period of 20 months (0 – 43) 51.6 % of patients experienced biopsy proven allograft rejection (at protocol or indication biopsy) that was treated with steroids, plasma exchange, high dose of intravenous immunoglobulins, antithymocyte globulin, or optimization of maintenance immunosuppression, depending on the type and stage of the rejection. 1-year death-censored graft survival was 94.8 % and 1-year patient survival was 93.5 %. 31 patients (20 %) acquired COVID-19 during the first postTX year and one of them died of severe COVID-19 at 6 months. Median creatininemia at 1 year was 114 μmol/L (56 - 299) (Table 1).
We observed only a 5.5 % decline in kidney TX rates as compared to equivalent time period before COVID-19 pandemic (155 vs 164 kidney TX or 4 vs 4.5 per month).
Conclusion: We sustained our TX program during the time of COVID-19 pandemics at almost same rate as before the pandemics and with satisfactory results, providing our patients the best renal replacement therapy even during the hard times.
[1] COVID-19 pandemic, Kidney transplantation, Survival
