Comparison of risk factors and outcome between high and low Cytomegalovirus viremia in living donor R+D+ renal transplant recipients from Pakistan
Sunil Kumar Dodani1, Asma Nasim1.
1Infectious Disease, Sindh Institute of Urology and Transplantation, Karachi, Pakistan
Introduction: Cytomegalovirus (CMV) infection after renal transplantation can cause graft dysfunction with morbidity and mortality. Our center is an exclusive living donor program with 99% R+D+. Due to non-availability and cost of oral valgancylovir, we do not give prophylaxis rather opt for event driven CMV treatment. Our aim is to identify risk factors and outcome in patients with high CMV viremia so that we can select them for prophylaxis in the background of financial and logistic constraints.
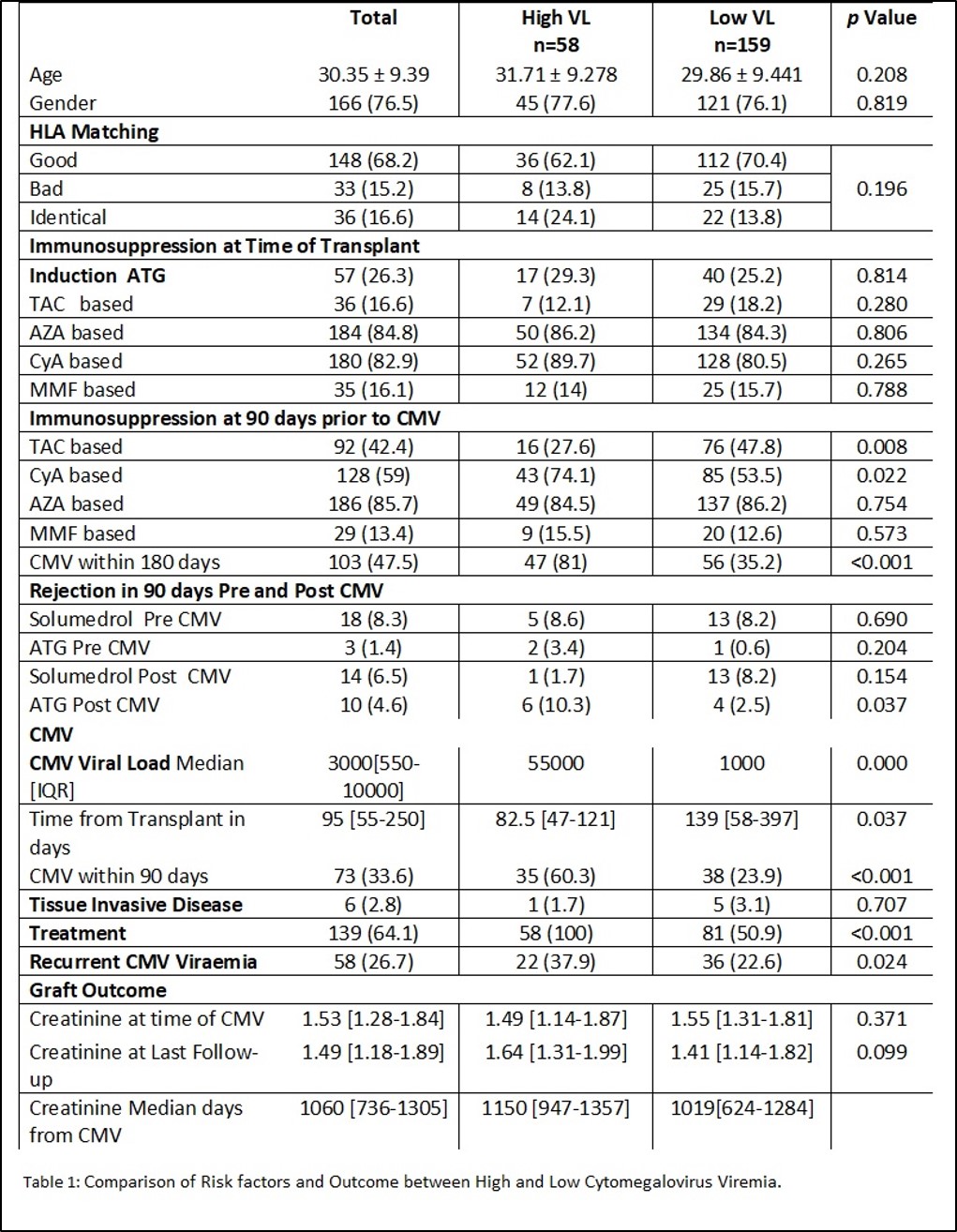
Methods: The files of renal transplant recipients who receive graft from January 2018 to December 2020 are reviewed. The first CMV episode is taken. High viral load is defined as >104 IU/ml. Demographics, HLA match, time since transplant, immunosuppression at the time of transplant and 90 days before CMV episode, rejection 90 days before and after CMV episode, tissue invasive disease, recurrent CMV and serum creatinine at the last follow up (4 years post-transplant) are compared between high and low viral loads.
Results: A total of 336 files are reviewed. Out of these 217 (64.5%) developed CMV Viremia, with 37% within 90 days. Fifty eight (26.7%) had high viral load. The median high viral load is 55000 IU/ml and low viral load is 1000 IU/ml. A total of 184 (84.7%) had good match. Age, gender, HLA match and immunosuppression at the time of transplant are comparable between high and low viral loads. Patients developed high CMV viremia significantly early post-transplant (median days 82 vs 139 p=0.037). Cyclosporine and tacrolimus are associated with CMV. Six (2.7%) patients develop tissue invasive disease with no difference in viral load. Overall there are 45 (8.7%) episodes of acute rejection within 90 days pre and post CMV infection with no difference between high and low viral loads. Subsequent CMV episodes are significantly high among patient with high viral load, however there is no significant difference in serum creatinine at the last follow-up.
Conclusion: One third of patients develop CMV viremia within 90 days post-transplant. High viral load is observed early post-transplant. There is no difference in rejection episode or graft function between high or low viremia. Only 2.7% develop tissue invasive disease. Event driven CMV treatment in our center seems an appropriate strategy; however, more studies are required to validate our findings.
[1] Cytomegalovirus
[2] living donor
[3] renal transplant
