Deep cutaneous fungal infections in kidney transplant recipients
Abdullah Ansari1, Anupma Kaul1, Rungmei Marak2, Manas Behera1, Narayan Prasad1, Dharmendra Bhadauria1.
1Nephrology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India; 2Microbiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India
Introduction: Kidney transplant recipients are at increased risk of opportunistic infections. Deep cutaneous fungal infections (DCFI) are varied in transplant recipients, but there is a paucity of data regarding them. It is pivotal to characterize these infections for early diagnosis and treatment initiation; thus, limiting potential fungal dissemination.
Method: A 15-year retrospective observational study from January 2007 to December 2021 at a tertiary center in northern India. The relevant clinical data on transplants, fungal species, treatments, and outcomes were studied from electronic records. The cases were selected if they had specimens available from lesions for Culture or Histopathology.
Results: Deep cutaneous fungal infections were diagnosed in 52 (3.15%) patients among 1649 patients. The majority of patients were males (n=49, 94.2%). All donors were living, 22 (42.3%) related, and 30 (57.7%) unrelated including 28 spousal donors. 5 (9.6%) transplants were ABO-incompatible. One patient had a second transplant. Regarding induction, 21 (40.4%) received Basiliximab, 11 (21.2%) received Thymoglobulin and 20 (38.3%) didn't receive any induction. The associated comorbidities included Diabetes (57.7%, n=30), CMV infection (3.8%, n=2), hepatitis-B (5.8%, n=3), and hepatitis-C (7.7%, n=4), prior rejections (38.5%, n=20) and chronic renal allograft injury (32.7%, n=17). DCFI occurred at a median of 15.5 (IQR 6.25-25.75) months post-transplantation. The mean age and mean serum creatinine at diagnosis were 42.83 ± 11.65 years and 1.70 ± 0.88 mg/dl, respectively. The lesions predominated on the lower limbs (n=35, 67.3%) followed by the upper limbs (n=11, 21.2%). The lesions were polymorphic: nodules or papules (n = 40, 76.9%), abscess (n = 6, 11.5%), ulcerated or necrotic lesions (n = 3, 5.8%), or other [proliferative lesion (n = 2), blisters (n = 1)]. 3 (5.8%) patients had disseminated disease. All specimens obtained from lesions were positive for histopathology and 38 (73.1%) lesions were culture positive also. The most frequent infection was Phaeohyphomycosis (84.6%, n=44), followed by Aspergillosis (7.7%, n=4), Candidiasis (3.8%, n=2), Mucormycosis (1.9%, n=1) and other Hyalohyphomycosis (1.9%, n=1). All of them received systemic antifungal therapy [Itraconazole (n=37, 71.2%) Voriconazole (n=8, 15.4%)], and the immunosuppression was reduced simultaneously. 30 (57.7%) patients required surgical excision. One patient with disseminated Mucormycosis died during hospitalization. During a median follow-up of 58 months; 15 (28.8%) patients died, 8 (15.4%) relapsed, and 2 (3.7%) had graft loss. All mortality causes were unrelated to DCFI, bacterial sepsis being the most common.
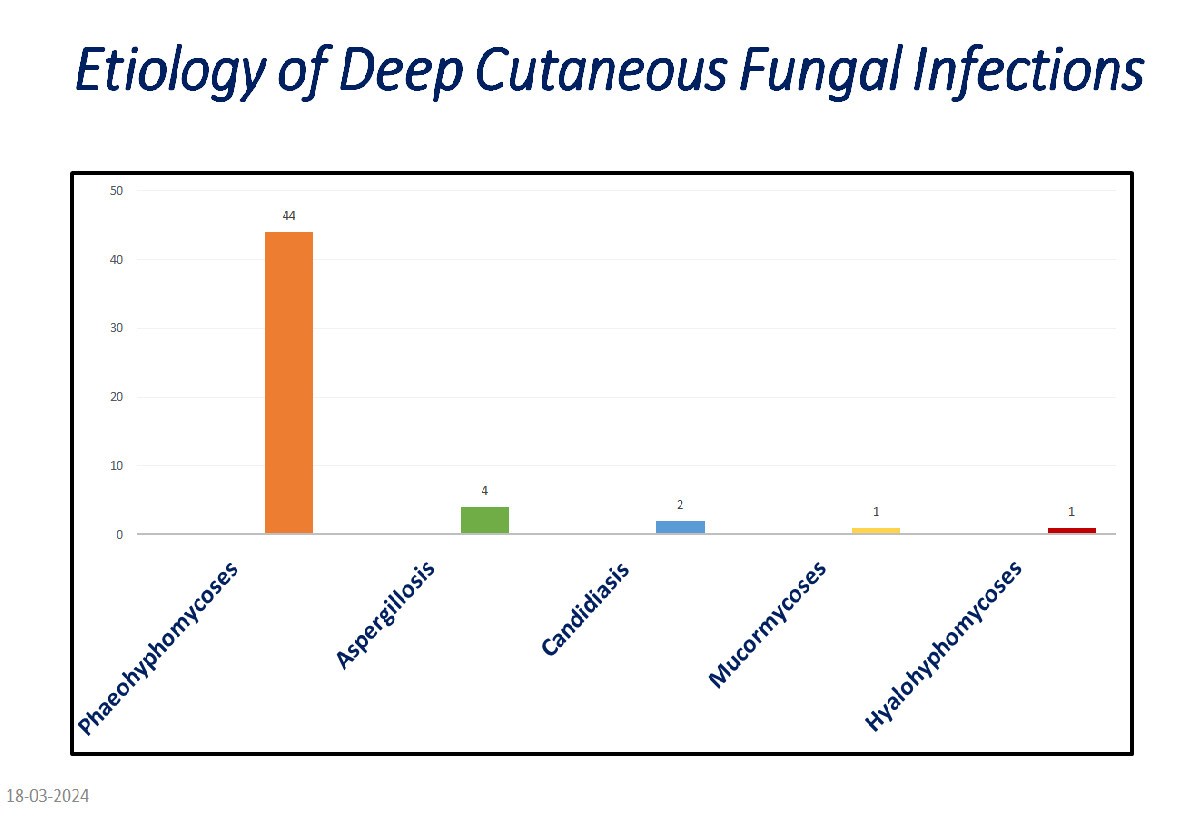
Conclusion: Phaeohyphomycoses were the most frequently observed DCFI. A high index of suspicion is required in transplant recipients with chronic indolent skin and subcutaneous swellings. Antifungal therapy with/without surgical excision results in complete resolution in most patients.
None.
[1] kidney transplant
[2] fungal infection
[3] deep cutaneous
