
Panel reactive antibody levels decline with increasing age: potential of augmented organ availability and improved outcomes for sensitized older recipients
Friederike Martin1,2, Elizabeth Zicari1, Merih Gizlenci1, Yao Xiao1, Keita Nakamori1,3, Yuko Sato1, Hao Zhou1, Edgar L. Milford4, Melissa Y. Yeung4, Stefan G. Tullius1.
1Division of Transplant Surgery, Department of Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, United States; 2Department of Surgery, Campus Charité Mitte | Campus Virchow-Klinikum, Charité - Universitätsmedizin, Berlin, Germany; 3Department of Urology, Osaka Medical and Pharmaceutical University, , Osaka, Japan; 4Department of Medicine, Renal Division, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, United States
Introduction: Sensitization against HLA (human leucocyte antigens) in patients waiting for transplantation challenge organ allocation, augment alloimmunity and lead to inferior outcomes. We hypothesized that calculated panel-reactive antibodies (cPRA) decline with age and delineated the relationship between age and sensitization levels among patients waitlisted for deceased donor kidney transplants. An experimental transplant model was utilized to define dynamics of sensitization across differing donor/recipient combinations emphasizing on delineating the role of recipient age.
Method: 483,793 patients waitlisted between 01/01/2009 and 06/30/2023 in the US for deceased donor kidney transplants registered in the UNOS Standard Transplant Analysis and Research file (2023) have been analyzed. Dynamics of maximum cPRA reported for each waitlisted patient were calculated. Data analysis was conducted using JMP®, Version 16.2.0, SAS Institute Inc., Cary, NC USA.
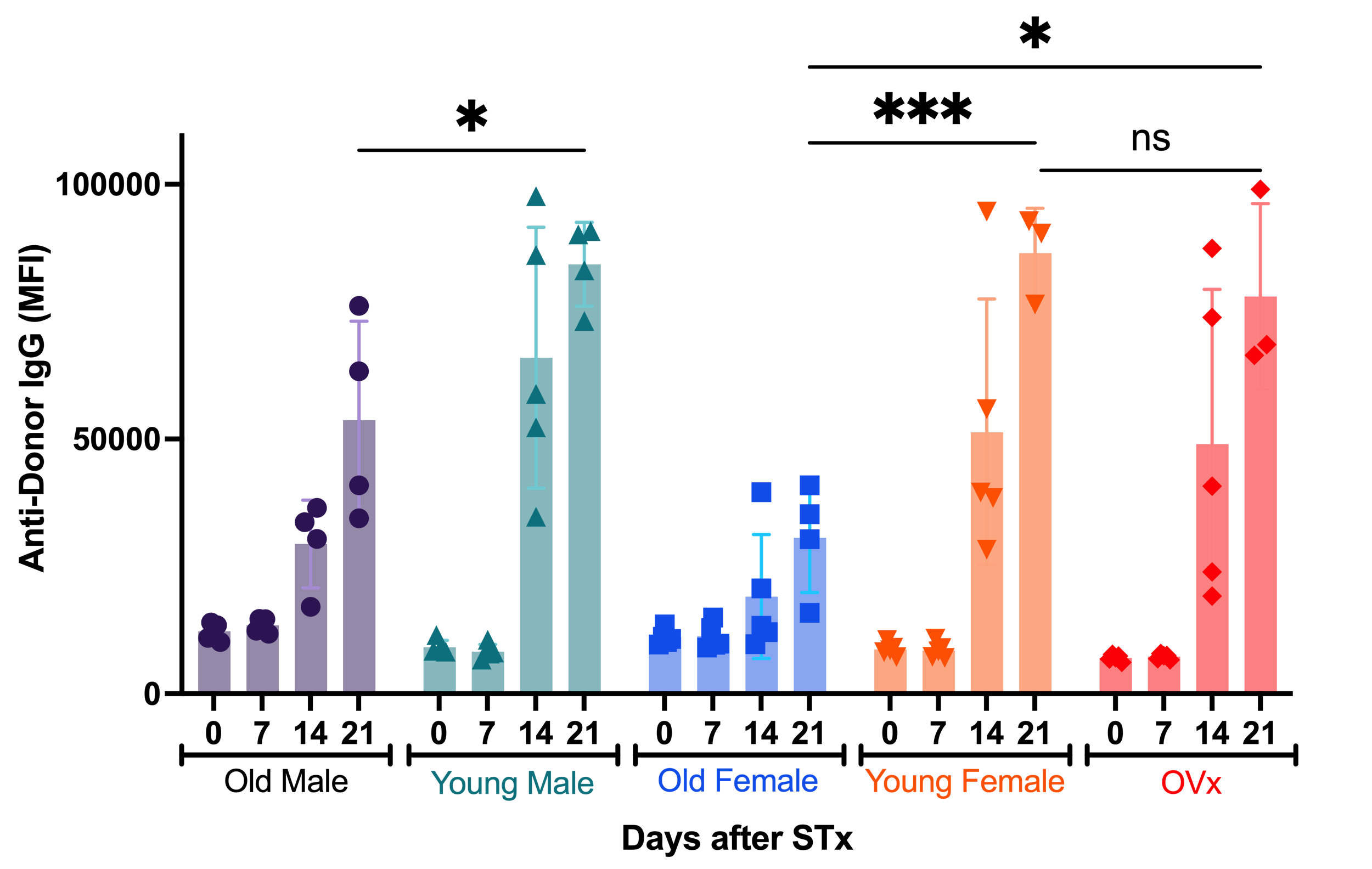
To further analyze the effects of aging on sensitization, we made use of young and old female and male C57BL/6 mice (3 and 20 months, respectively), that underwent fully MHC mismatched skin transplants from either female or male young DBA/2 mice; an additional group of young female animals underwent ovariectomies prior to transplant. Recipient serum was collected at serial intervals (end of the observation period by day 21); anti-donor IgG levels were measured by flow cytometry.
Results: Increasing recipient age resulted into reduced rejection rates and prolonged death-censored graft survival (9.7 years vs. 11.5 years in recipients 20-30 vs. 60-70 years old). These trends remained consistent irrespective of recipient sex. Notably, with increasing patient age, cPRA declined among waitlisted patients. While 22% of patients aged 20-30 years were highly sensitized (cPRA ≥80%) only 12% of the 60–70 years old patients presented with a cPRA ≥80%. This trend was particularly evident in patients who underwent a previous transplantation (Figure 1).

Experimentally, we observed declining IgG antibody levels in old mice after transplant (Figure 2). This effect was particularly pronounced in female recipients (mean MFI in old females 30,590 ±10,732 vs. 86,494 ± 8,823 in young females by day 21, p<0.0001). Of note, estrogen deprivation in young female animals did not affect sensitization levels.
Conclusion: Clinically, we observed a decline in maximum reported cPRA with increasing patient age, particularly notable in individuals with a history of prior transplantation. Experimentally, we have shown decreased anti-donor IgG levels in old recipients. Those data suggest that improved graft survival and reduced rejection rates with advancing recipient age are, at least in part, driven by an ameliorated humoral immune response.
[1] Panel Reactive Antibodies
[2] Aging
[3] Sensitization
[4] Donor-Specific Antibodies
