Follow the leader: HLA-B leader dimorphism predicts long-term survival following lung transplantation
Steven Hiho1,2, Andrew Brooks3, Bronwyn Levvey2, Mary Diviney1, Gregory Snell2, Glen Westall2, Lucy Sullivan2,3,4.
1Victorian Transplantation and Immunogenetics Service, Australian Redcross Lifeblood, Melbourne, Australia; 2Lung Transplant Service, Department of Respiratory Medicine, The Alfred Hospital, Melbourne, Australia; 3Department of Microbiology and Immunology, University of Melbourne at the Peter Doherty Institute for Infection and Immunity, Melbourne, Australia; 4South Australian and Immunogenetics Service, Australian Redcross Lifeblood, Adelaide, Australia
Introduction: HLA-B leader sequence peptides modulate T- and Natural killer (NK) cell responses via the expression of HLA-E. A sequence dimorphism in exon 1 of the HLA-B leader encodes a methionine (Met; M) or threonine (Thr; T) giving rise to 3 HLA-B leader genotypes: TT, MT or MM. Previous studies have shown that the HLA-B leader genotype influences outcomes following hematopoietic cell transplantation (HCT), whereas the impact of HLA-B leader on solid organ transplantation is unknown. The aim of this retrospective study was to investigate the role of this HLA-B leader sequence on long-term outcomes following lung transplantation.
Method: We retrospectively analysed HLA-B leader sequences in 310 primary adult lung transplant recipients and donors transplanted between 2008 and 2015. Sequencing was performed by next generation sequencing (NGS) and the HLA-B leader sequence peptides for both recipients and donors were defined as MM, MT or TT and either “matched” or “mismatched” was determined. Primary outcomes measured were chronic lung allograft dysfunction (CLAD) and overall survival. Cox regression and survival curves were calculated to assess associations.
Results: Recipient B leader peptide frequency in our cohorts were MM=14%. MT=29% and TT=47%, while donor frequencies were MM=9%, MT=41% and TT=50% respectively. HLA-B leader mismatching did not associate with either rejection [1.03(0.75,1.42) p=0.881] or overall survival [0.87(0.60,1.25) p=0.442] following LTx in multivariate cox regression models. Intriguingly however, donor HLA-B MM leader genotype alone associated with increased overall survival [0.39(0.15,0.99) p<0.05] after adjustments for other risk factors. Lung transplant recipients who received an allograft from donors carrying the HLA-B MM genotype demonstrated longer overall survival when compared to either MT or TT genotypes (Figure 1).
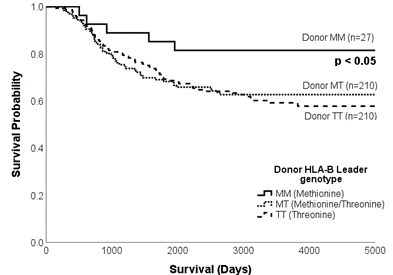
Conclusion: Here, we demonstrated for first time that HLA-B leader genotypes can influence outcomes following solid organ transplantation. Specifically, donor MM genotype was associated with improved overall survival following lung transplantation. More work on larger cohorts is required to evaluate what mechanisms are involved in this process. However, using HLA-B leader sequences could be utilised as an extra tool for evaluating immunological risk in solid organ transplantation.
The Lungitude Foundation.
[1] HLA
[2] Lung transplant
[3] B leader
