Harm reduction approach: An ethical proposal for liver transplant recipients with alcohol-associated liver disease
Sue Hyon Kim1,2, Marina Serper3.
1School of Nursing, University of Pennsylvania, Philadelphia, PA, United States; 2Leonard Davis Institute for Health Economics, University of Pennsylvania, Philadelphia, PA, United States; 3Division of Gastroenterology and Hepatology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States
Introduction: Concerns regarding alcohol consumption after liver transplantation (LT) have prompted numerous studies conducted in accordance with recommendations for complete abstinence. However, this is situated amidst various ethical considerations, such as paternalism, stigmatization, and social determinants of health. This study supports the implementation of harm reduction as an ethical and pragmatic alternative for addressing post-LT alcohol use in recipients with alcohol-related etiologies. Ultimately, it aims to provide valuable insights into the application of harm reduction in LT clinical settings.
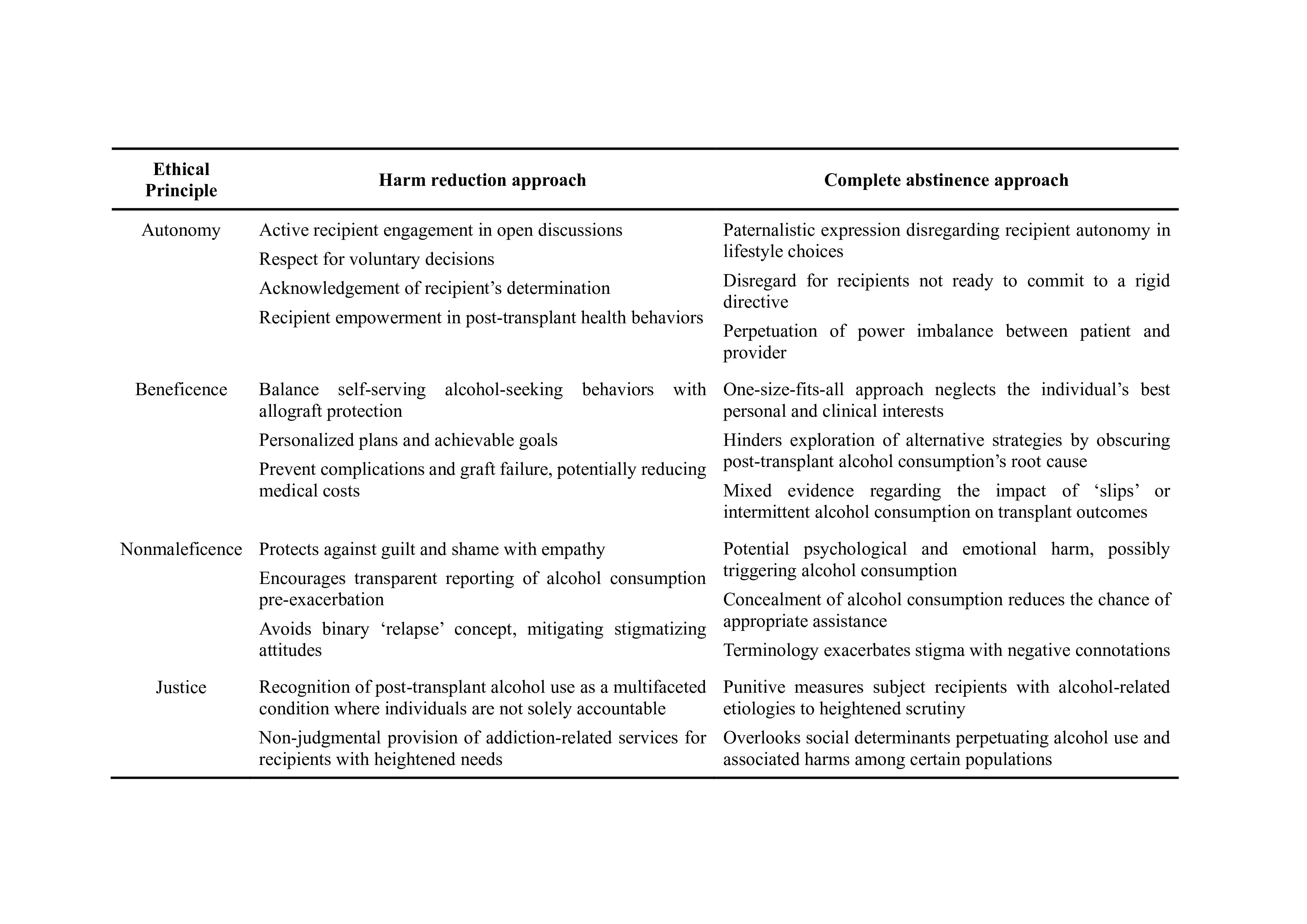
Method: The four principles of biomedical ethics (autonomy, beneficence, non-maleficence, and justice) were applied in the critical evaluation of the traditional complete abstinence approach and the proposed harm reduction approach. Potential controversies of harm reduction were also addressed, elucidating areas of consideration and initiatives for clinicians in this evolving landscape.
Results: The recommendation for complete abstinence after LT disregards the individual’s autonomy in making lifestyle choices. It fails to consider those who may benefit from gradual tapering or moderate alcohol use. LT recipients may feel compelled to conceal their alcohol consumption in fear of repercussions, delaying professional help. Additionally, the emphasis on drinking behavior overlooks associated social and structural factors, along with the fact that other indications for LT, such as nonalcoholic fatty liver disease, are also linked to personal actions. In contrast, harm reduction acknowledges post-LT alcohol use as a multifaceted condition where individuals cannot be held entirely responsible. This fosters open discussions between patients and providers, allowing for personalized care plans with realistic goals (Table 1). While seemingly counterintuitive and undermining professional judgment, harm reduction actually complements clinical expertise with a person-centered approach incorporating compassion and advocacy. Its application in other substance use disorder settings has also demonstrated increased treatment initiation without a corresponding rise in the risky behavior itself, thereby mitigating adverse consequences. As an approach supported by national and international bodies such as the WHO and CDC, harm reduction in LT is expected to benefit a broader range of recipients with varying degrees of alcohol dependence and maintain liver graft function without complications.
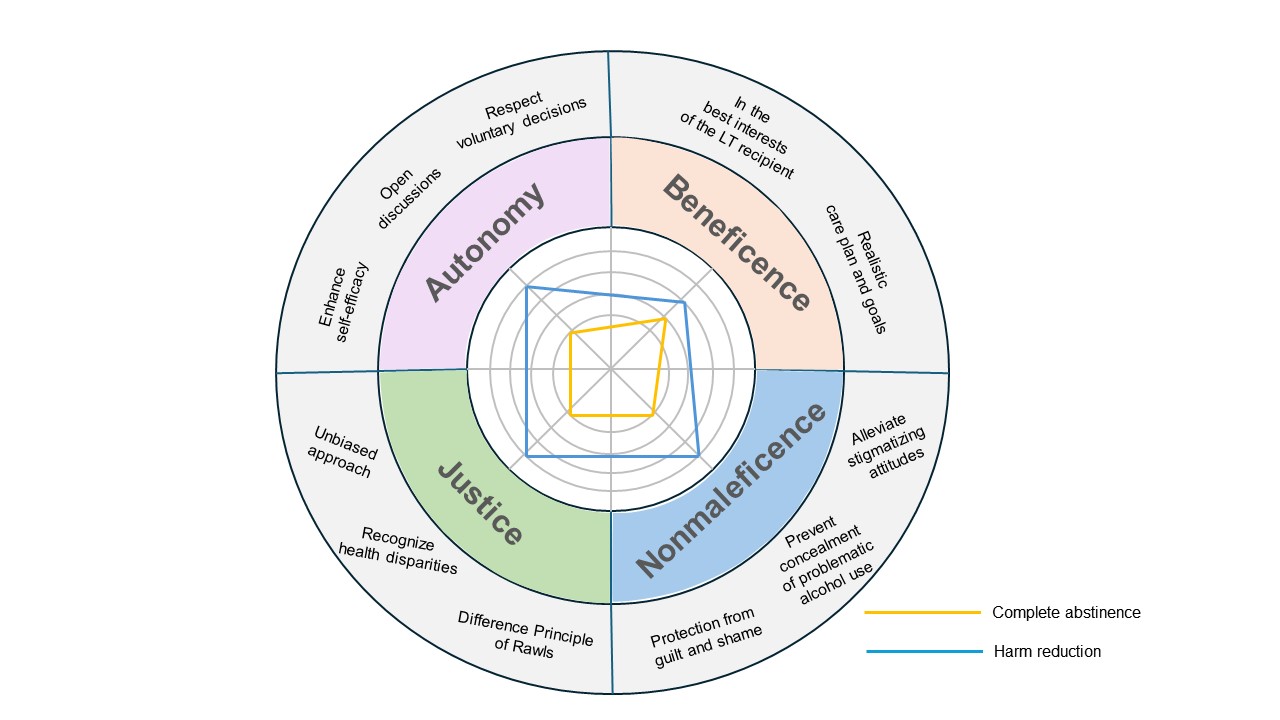
Conclusion: Compared to conventional abstinence-oriented approaches, harm reduction for post-LT alcohol consumption offers improved alignment with the four ethical principles in biomedicine (Figure 1), as well as positive clinical outcomes. Embracing the philosophy of harm reduction, clinicians must foster an environment of mutual respect, prioritize recipients’ best interests, diminish stigma, and guarantee equitable treatment for LT recipients with alcohol-related etiologies.
[1] Harm Reduction
[2] Liver Transplantation
[3] Alcohol-associated Liver Disease
[4] Alcohol Relapse
