A multicenter retrospective cohort study of indian experience with the kidney paired donation transplantation
Hari Meshram1,2, Vivek Kute2, Himanshu Patel2, Subho Banerjee2, Feroz Aziz3, Suraj Godara3, Shyam Bansal3, Anil K Bhalla3, Ashish Sharma3, Vishwanath Billa3, Priyadarshi Ranjan3, Manish Singla3, Sandeep Guleria3, Deepak Ray3, Madan Mohan Bahadur3, Bharat Shah3, Aneesh Shrivastava3, Sanshriti Chauhan2, Jaydeep Hirpara3, Manish Balwani3, ISOT Kidney exchange group3.
1Nephrology, ILBS, Vasant Kunj, New Delhi, New Delhi, India; 2Nephrology, IKDRC-ITS, Ahmedabad, Ahmedabad, India; 3ISOT-Kidney exchange study group, India, India
Introduction: In a living donor kidney transplantation (LDKT) dominated transplant program, kidney exchange may be a cost-effective and valid alternative strategy to increase LDKT in countries with limited resources where deceased donation kidney transplantation (DDKT) is in the initial stages.
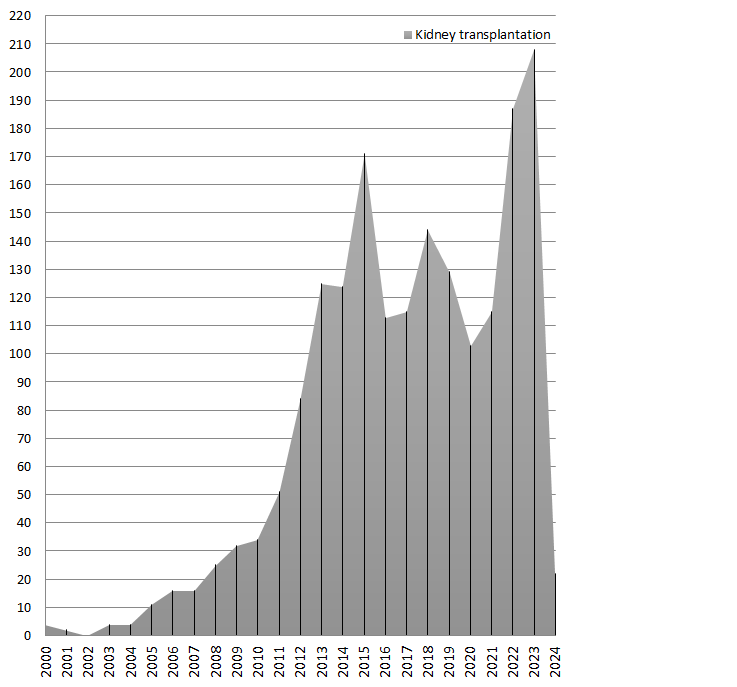
Methods: Here, we report a largest multicenter retrospective cohort study of Indian experience with 1839 kidney paired donation (KPD) transplantation in 65 centers over two decades
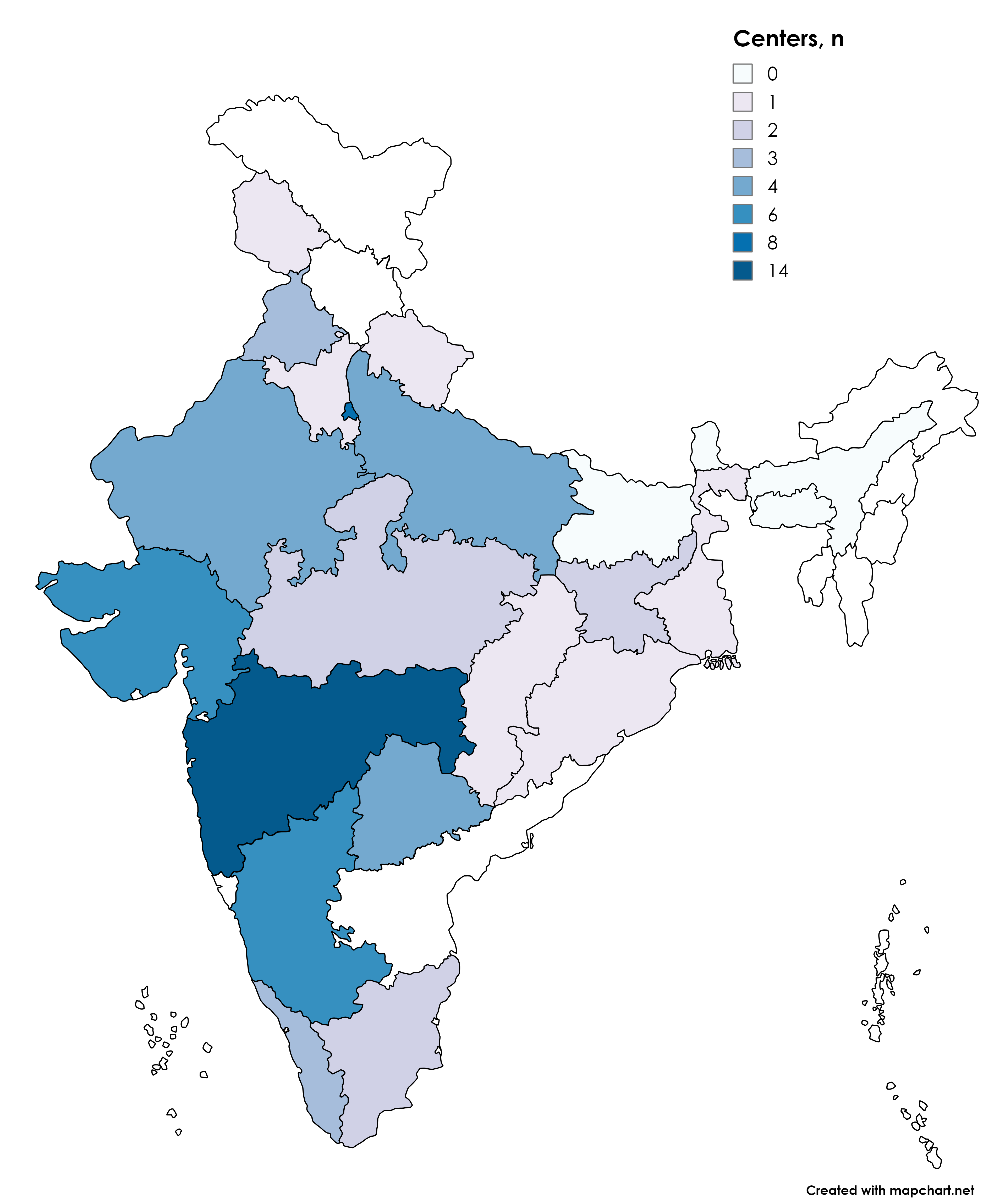
The study has been reviewed by the ethics committee and has therefore been performed in accordance with the ethical standards laid down in the Declaration of Helsinki as well as the Declaration of Istanbul. Near related donors (parents, spouse, sibling, children and grandparents) can be donor in KPD in India. Top single center reported 29% KPD transplants of this cohort. Top 5, 10, 20 and 25 centers performed 54 %, 73.5% , 87.3% and 90.6% of the KPD transplants. 16 and 10 centers have performed only one and two pairs of KPD transplants.
Gujarat (N=565), Maharashtra (N=220), Delhi (N=216), Kerala (N=155), Rajasthan (N=141) were top States for KPD transplants. Majority of KPD was with manual allocation rather than software due to resource limitations.
Results: Most common reason for joining KPD among transplanted patients was ABO incompatibility in 9 out of 10 patients. More than 3/4th cases of KPD were two-way exchanges with simultaneous surgery. There was overwhelming preponderance of female donors and male recipients but similar to our respective LDKT program. The graft survival, patient survival, biopsy-proven rejection rate, and graft function was similar to other LDKT outcomes in historical cohort. All were single center KPD except few multicenter inter-hospital city based (n=107) KPD. Mumbai (N=66) and Kozhikode (N=27) are tops city for multicenter KPD. Other special features were 10 KPD transplants in single day and longest 10-way KPD at Ahmedabad, intercity with donor travel exchanges (n=4), international exchanges from near related donors (N=6).
Conclusion: Our largest multicenter KPD cohort study support that although KPD is medically simple but underutilised due to beurocratically complex logistics. Government should promote multicentre and National KPD program with ease of doing KPD using single window registration, allocation and legal clearance to reduce waiting time in DDKT. We report largest multicenter cohort of KPD transplants in India and Asia.
