Portal venous repopulation of decellularised rat liver scaffolds with syngeneic bone marrow stem cells
Zeeshan Afzal1, Mekhola Hoff1, Simon Harper1, Emmanuel Huguet1.
1Department of Surgery , University of Cambridge , Cambridge, United Kingdom
Introduction: Liver transplantation is the only life-saving treatment for end-stage liver failure but is limited by the organ shortage and consequences of immunosuppression. Repopulation of decellularised scaffolds with recipient cells provides a theoretical solution, potentially allowing reliable and timely organ sourcing without immunosuppression. Recellularisation of the vasculature of decellularised liver scaffolds was investigated as an essential prerequisite to the survival of other parenchymal components, and with a focus on Liver Sinusoidal Cells (LSECs) given their central role in global hepatic function.
Methods: Rat liver decellularisation was carried out by portal vein (PV) perfusion using a detergent-based solution. Scaffolds were perfused via the PV with culture medium within an organ chamber at 37°C and infused with 107 primary bone marrow (BM) stem cells selected by plastic adherence. BM stem cells were assessed for key marker expression using fluorescence-activated cell sorting (FACS), and recellularised scaffolds analysed by light (LM), electron (EM) and immunofluorescence (IF) microscopy.
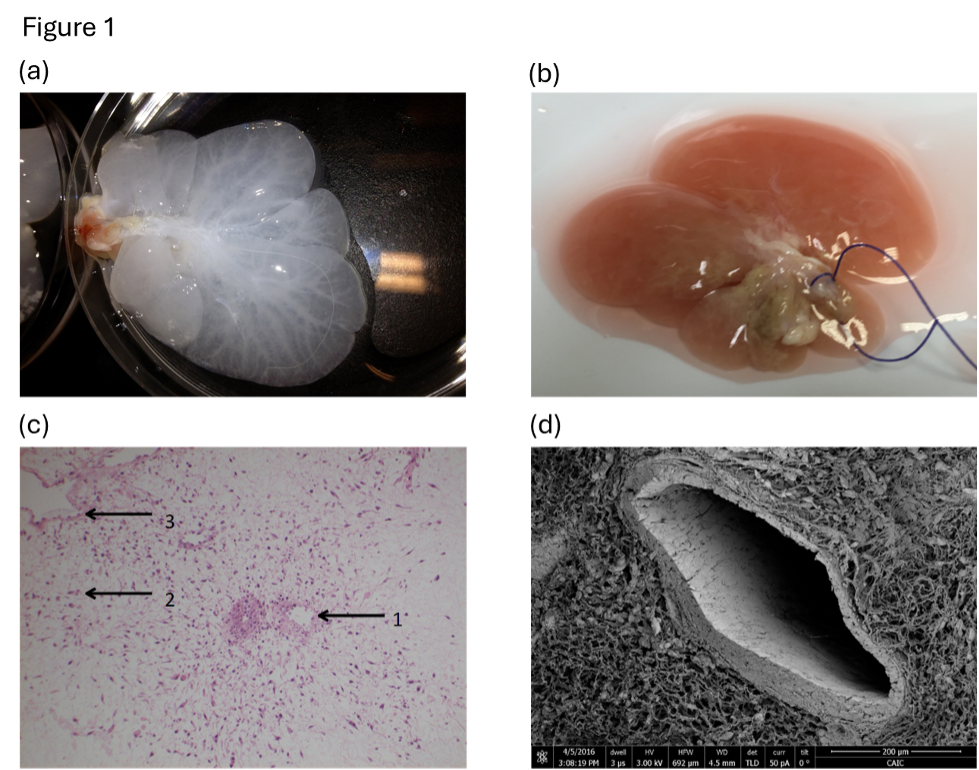
Results: Recellularised scaffolds changed in macroscopic appearance from a translucent (figure 1a) to an opaque (figure 1b) structure by day 30. Stem cells engrafted in portal, sinusoidal and hepatic vein compartments on LM (Figure 1c) with cell alignment reminiscent of endothelium on EM (Figure 1d). Engrafted cells expressed LSEC endocytic receptors (mannoseR, FcR and stabilinR), and cell surface marker expression altered following engraftment from a haematopoietic (CD31- CD45+) to an endothelial phenotype (CD31+ CD45−) on FACS and IF.
Conclusions: To our knowledge this is the first report of BM stem cells used to repopulate decellularised liver vasculature. This approach is potentially clinically relevant as the cells are recipient specific, sourceable in relevant numbers, and not subject to oncogenic concerns that relate to cell lines or induced pluripotent stem cells. These results represent one step towards complete recellularisation of liver vasculature and progress in generation of transplantable neo-organs.
