The impact of living kidney donation in a kidney exchange programme on the donor's health-related quality of life
Stijn Laar1,2, Berwout Wiltschut1, Chris Oudmaijer1, Kelly Muller1, Emma Massey3, Robert Porte1, Frank Dor2,4, Robert Minnee1.
1Department of Surgery, Division of HPB & Transplant surgery, Erasmus Medical Center Transplant Institute, University Medical Center Rotterdam, Rotterdam, Netherlands; 2Imperial College Renal and Transplant Centre, Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, Netherlands; 3Department of Internal Medicine, Nephrology and Transplantation, Erasmus Medical Center Transplant Institute, University Medical Center Rotterdam, Rotterdam, Netherlands; 4Department of Surgery and Cancer, Imperial College London, London, United Kingdom
Kidney exchange programs (KEP) have revolutionized living donor kidney transplantation (LDKT) by increasing the donor pool and enabling transplants for patients with incompatible donors. However, the implications for donors participating in KEP, particularly regarding postoperative health-related quality of life (HRQoL), are not well elucidated. This study aims to compare the mental and physical health outcomes of donors participating in KEP with donors who donate directly (non-KEP) using various health outcome measures over varying postoperative periods.
The study included 724 donors, with 167 in the KEP group and 557 in the non-KEP group. Outcomes were assessed using the mental component summary, physical component scale, self-rated EQ-5D-3L visual analogue score, MVI-20 score for fatigue, and self-rated pain level. The study found no significant differences in gender and age between the two groups, whereas donor type and methods of donor nephrectomy varied significantly.
Results indicated no significant difference in the mental and physical components between KEP and non-KEP donors in the initial postoperative period. However, as time progressed, certain periods showed significant variances in HRQoL measures, with some pointing to significantly better outcomes in the KEP group. After 1-year, the HRQoL was not different between both groups.
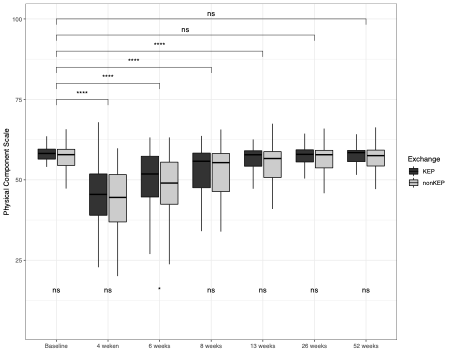
After propensity score matching, there were no significant differences in the SF-36 (MCS and PCS) between the KEP and non-KEP groups within the first year post donation.
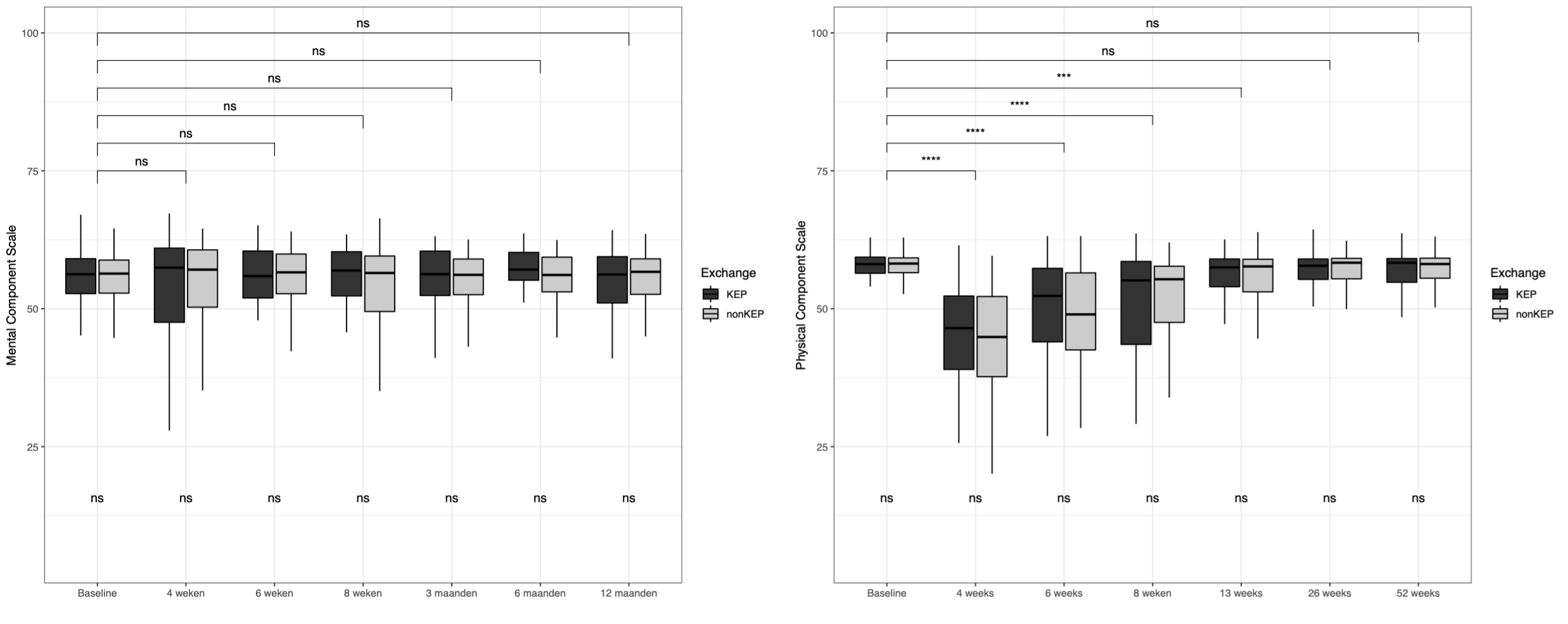
These results were comparable for the self-rated HRQoL (EQ-5D-3L) and the fatigue score (MVI-20) as well.
This study's findings suggest that participation in a KEP does not adversely affect donors' short- or long-term mental and physical HRQoL outcomes. With the increasing frequency of KEPs, these insights are reassuring, indicating that donors who participate in such programs can expect HRQoL comparable to those who do not. This reinforces the viability of KEP as a safe option for expanding LDKT and findings can inform patient and donor education. Future research should focus on longitudinal studies to assess the sustained impact of donor participation in KEPs on HRQoL.
[1] Living donation
[2] Kidney transplantation
[3] Health related quality of life
[4] Kidney Exchange Program
