Variation in global living donor liver transplant surgical technique: Early data from the International Living Donor Liver Transplant Registry
Ilya Kantsedikas1,3, Meera Raja2,3, Thomas Fernandez4,5, Toby Lewis6, Michael Spiro2,3, Dimitri Raptis7, Marina Berenguer8, Mohamed Rela9.
1Anaesthesia, Great Ormond Street Hospital, London, United Kingdom; 2Anaesthesia, Royal Free Hospital, London, United Kingdom; 3Department of Surgical Biotechnology, University College London, London, United Kingdom; 4Anaesthesia, Auckland City Hospital, Auckland, New Zealand; 5Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand; 6Critical Care, Royal London Hospital, London, United Kingdom; 7Organ Transplant Center of Excellence, King Faisal Specialised Hospital and Research Center, Riyadh, Saudi Arabia; 8Hepatology, La Fe University and Polytechnic Hospital, Valencia, Spain; 9Institute of Liver Disease and Transplantation, Dr Rela Institute and Medical Centre, Bharat Institute of Higher Education and Research, Chennai, India
LDLTregistry.org Collaborators.
Background: The International Living Donor Liver Transplant Registry (LDLTregistry.org) aims to address the evidence gap in living donor liver transplantation (LDLT) by collecting peri-operative data including outcomes from consecutive LDLT cases performed worldwide. Our description of variation in global LDLT practice is derived from LDLTregistry.org data collected from 1st September 2023 until 16th February 2024.
Methods: LDLTregistry.org is a prospective international registry intended to capture consecutive LDLT donor-recipient paired data. Data are captured using a specially designed platform (https://ldltregistry.org). Submissions from five months since the Registry opened were examined for variation in global LDLT practice by region (Africa, Asia, Europe, Middle East, North America and South America).
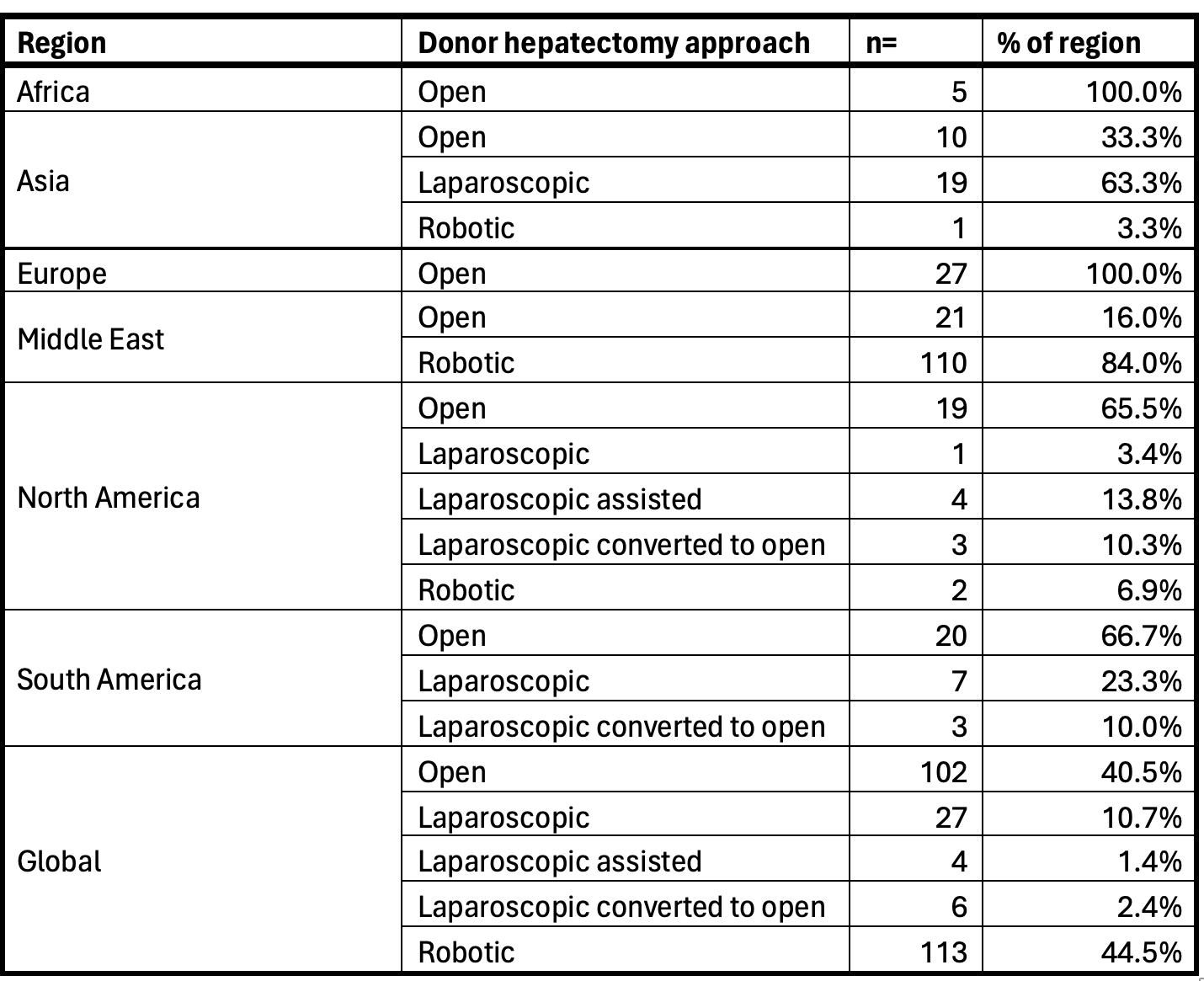
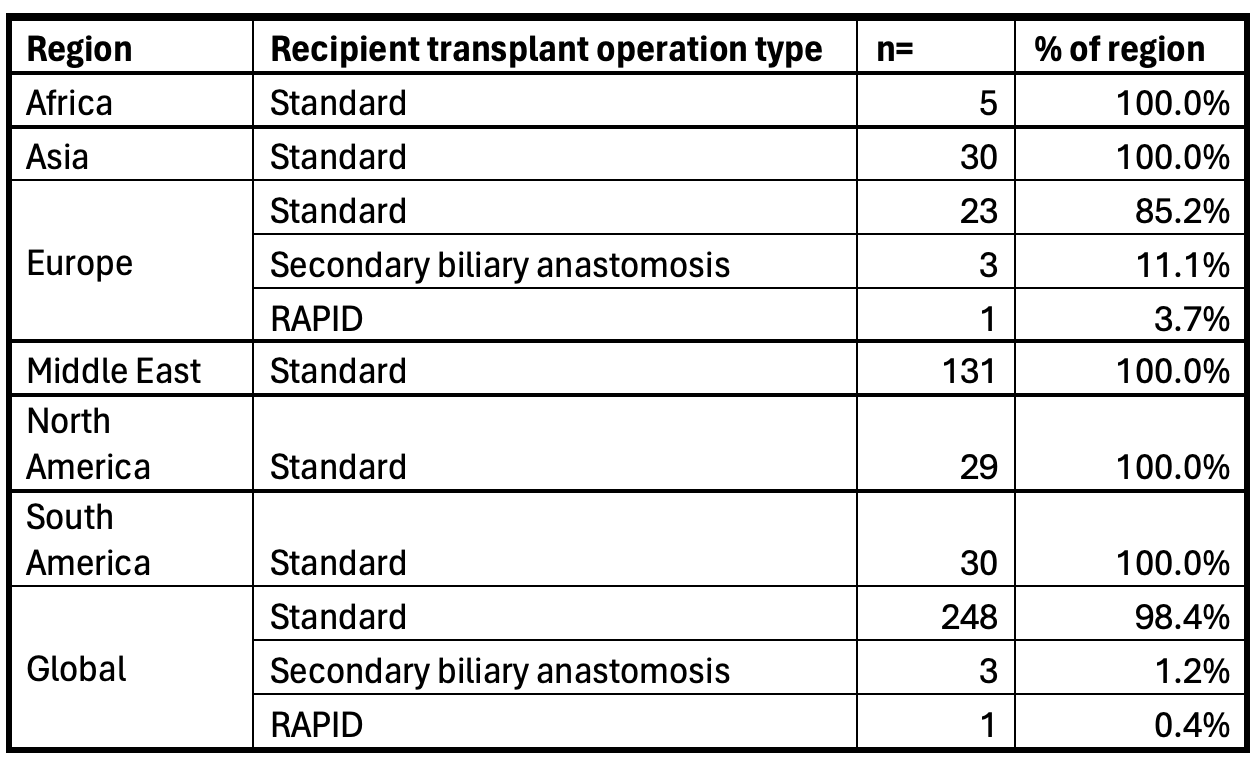
Results: A total of 504 cases (252 donor-recipient pairs) were examined. There was heterogeneity in donor hepatectomy technique (see table 1) with robotic approach most common among the cases reported to LDLTregistry.org, followed closely by open surgery. Majority of the robotic donor hepatectomies submitted to the Registry were performed in the Middle East, with a single centre accounting for 110 (43.6% of all submissions and 97.3% of robotic submissions). 98.4% (n= 248) of recipients had a standard transplant with a breakdown of the remainder shown in table 2.
Conclusions: This is a limited examination of early data from LDLTregistry.org showing variations in LDLT practice. The Registry captures a considerably broader dataset and will examine donor and recipient outcomes and factors that influence them. A more detailed analysis of the Registry data including outcomes will be published. We encourage consecutive case submissions to LDLTregistry.org to build the evidence base for improving global LDLT practice.
[1] living donor liver transplant
[2] LDLT
[3] donor hepatectomy
[4] living liver donor
