A liver for a kidney: Donor and professional attitudes toward trans-organ exchange
Elizabeth Nies1, Bhabna Pati1, Esra Alagoz1, Benjamin Samstein2, Jonathan M Cullen3, John P Roberts4, Carrie Thiessen1.
1Department of Surgery, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; 2Department of Surgery, Weill Cornell Medical College, New York, NY, United States; 3Department of Surgery, The University of Texas Health Science Center at San Antonio, San Antonio, TX, United States; 4Department of Surgery, University of California San Francisco, San Francisco, CA, United States
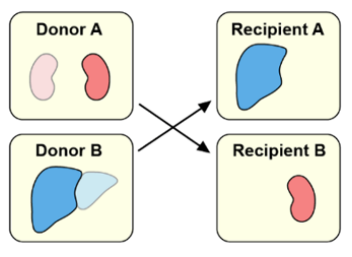
Introduction: Due to a shortage of available organs for transplant, many individuals with end-stage renal or liver disease die while on a waiting list. A liver-for-kidney exchange (LFKE) is a rarely performed paired exchange in which one donor donates a liver while another donor donates a kidney. In exchange, each recipient receives their needed organ (Figure 1). Some donors with organ-specific reasons for ineligibility could give a different organ than originally intended, thus increasing the number of living donors, potentially ameliorating the organ shortage. This study characterizes ineligible donor and transplant professional attitudes toward and concerns about LFKE.
Methods: Ineligible living kidney and liver donors, and transplant professionals from high-volume US transplant centers completed 45-minute-long semi-structured interviews. Interviews included a deliberative briefing on LFKE. Interviews were audio-recorded, transcribed, de-identified, and analyzed using NVivo. We employed an inductive approach to identify themes.
Results: Ten people participated in our study: one ineligible living liver donor, four ineligible living kidney donors, two nephrologists, one hepatologist, one transplant coordinator, and one surgeon. Overall, participants were receptive to LFKE. Some donors were not personally interested in LFKE but still supported the concept.
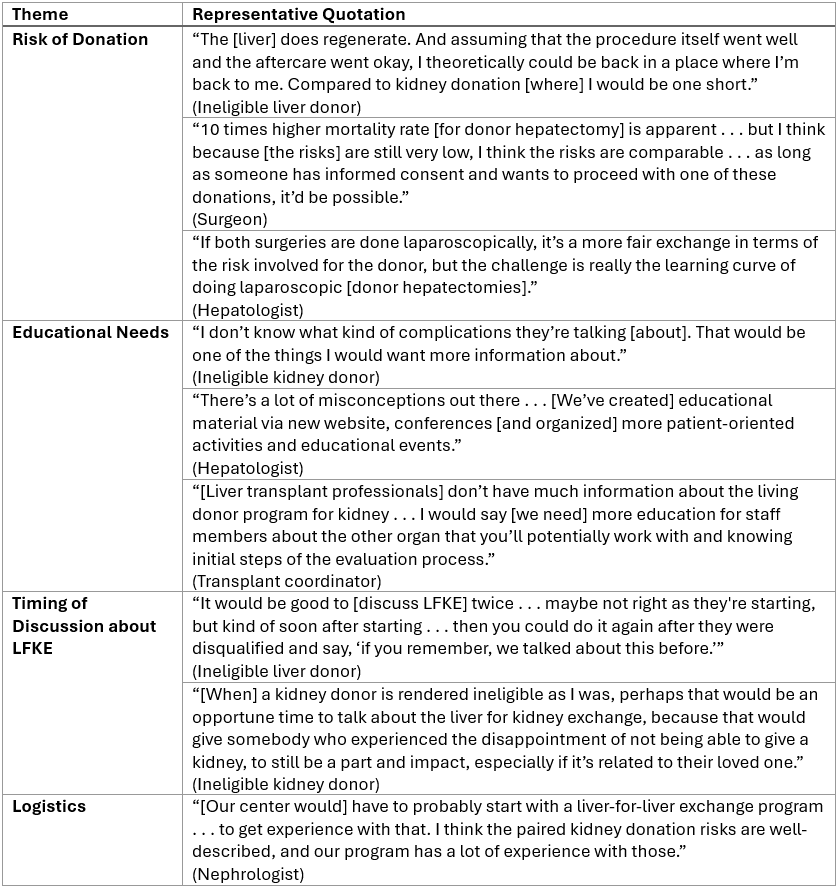
Theme 1: Risk of donation. Both patients and transplant professionals carefully evaluated short-term and long-term risk (Table 1). While the ineligible living liver donor was unwilling to take greater long-term risk of kidney donation, the ineligible kidney donors were willing to take on the greater short-term risks of donor hepatectomy. Professionals noted the lack of information about the long-term risks of kidney donation and discussed potential changes to clinical practice that could minimize the risk differential in LFKE.
Theme 2: Educational needs. Ineligible kidney donors were open to living liver donation if they had more information on specific complications of donor hepatectomy their management. Professionals voiced their need for more education on the evaluation and transplant process of the opposite organ to better counsel potential LFKE donors.
Theme 3: Timing of discussions about LFKE. Some donors would prefer that transplant professionals bring up LFKE early on in their evaluation while others would prefer to learn about LFKE after they are deemed ineligible for their initial organ.
Theme 4: Logistics. Professionals suggested expanding liver for liver exchange programs to improve the logistics of liver transplantation prior to establishing LFKE programs.
Conclusion: Both ineligible donors and transplant professionals were receptive to the possibility of LFKE. They carefully weighed the difference in risks between kidney and liver donation. Their comments highlighted informational content, timing, and logistical considerations relevant to centers who seek to establish LFKE programs.