
Organ donation after euthanasia in Spain: A summary of the first results
Alicia Pérez1, Javier J Sanchez1, Rebeca R Bajo1, Haizea H Olasagasti2, Gabriel Moreno3, Nuria N Masnou4, Teresa Pont5, Juan Araiz6, Rafael Badenes7, Fernando Martínez- Soba8, Beatriz Domínguez-Gil1.
1Deceased donation , Organización Nacional de Trasplantes , Madrid, Spain; 2Donor coordinator, Osakidtza, Vitoria, Spain; 3Donor coordinator, Hospital Univ. de Bellvitge, Barcelona, Spain; 4Donor coordinator, Hospital Univ. Doctor Josep Trueta, Gerona, Spain; 5Donor coordinator, Hospital Univ. Vall d´Hebrón, Barcelona, Spain; 6Donor coordinator, Hospital Clínico Univ. Lozano Blesa, Zaragoza, Spain; 7Donor coordinator, Hospital Clínico Univ. de Valencia, Valencia, Spain; 8Donor coordinator, Hospital San Pedro, La Rioja, Spain
Background: The euthanasia law entered into force in Spain in July 2021. A national protocol on organ donation after euthanasia (ODE) was officially adopted in July 2022. The guidance emphasizes that euthanasia should be prioritized over donation being the patient’s comfort paramount.
Objective: To describe the experience on ODE in Spain.
Method: A retrospective study of cases of ODE performed since August 2021 to December 2022 and the post-transplant outcomes of the thoracic organs.
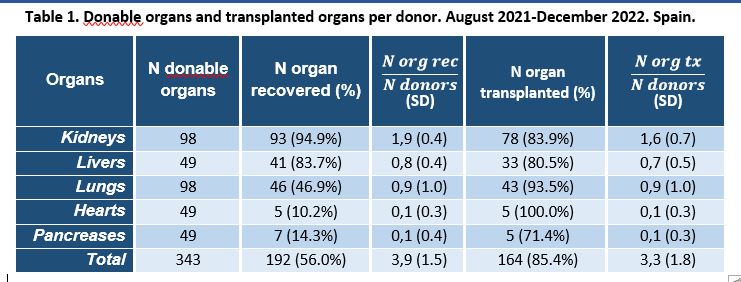
Results: In total, 49 patients donated organs after euthanasia, seven in 2021 and 42 in 2022. Donors were most frequently males (n=28; 57%) and mean age was 59.8 (SD: 10.6) years. Underlying diseases were amyotrophic lateral sclerosis (n=19; 39%), multi systemic atrophy (n=4; 8%), spinal cord injury (n=4; 8%), Alzheimer (n=3; 6%), multiple sclerosis (n=2; 4%), Parkinson (n=2; 4%) and other (n=15; 31%). All patients were directly admitted in the ICU (66%) or the ward (44%) except four who were transferred in a medicalized ambulance after receiving sedation at home. Patients were subsequently transfer to the operating theater where euthanasia medication was delivered and death declared. Of the 49 donors 96% were utilized donors. 135 transplant procedures were performed (69 kidney, 29 liver, 23 lung, 5 heart, 5 combined kidney-pancreas and 4 combined kidney-liver transplants). The mean organs retrieved per donor was 3.9 and the mean organs transplanted per donor was 3.3. Table 1
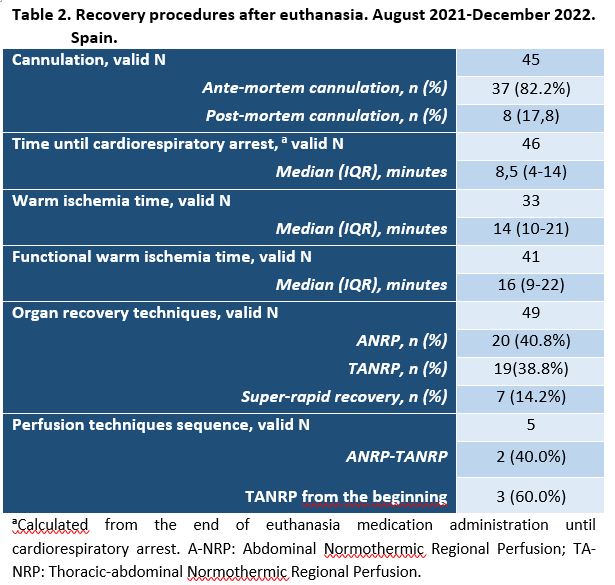
Organ recovery was based on abdominal (A-NRP) or thoracoabdominal normothermic regional perfusion(TA-NRP)(n=44; 90%) or standard rapid recovery (n=5; 10%). 2 hearts were recovered after the abdomen was perfused using A-NRP (an intra-aortic balloon occluding the iliac artery was previously inserted) while the 3 aortic arch vessels were vented. 3 hearts were recovered using TA-NRP (the 3 aortic arch vessels were previously vented) from the beginning of the procedure. Median time from administration of euthanasia medication to cardiac arrest was of 8.5 minutes (IQR 4-14). Table 2
Of the 131 recipients, mean age 57.4 (SD 12.3), (62.6%) were men. 2- year- heart survival is 80%. 1 of the heart recipients died at 28th post-transplant, due to pericardial tamponade. Of the 23 lung recipients, 7 (30.4%) presented primary organ dysfunction, of those two died at 6th month and another died at 12th post-transplant.
Conclusions: ODE is respectful with patient’s end-of-life plans and allows waitlisted patients to receive life-saving and life-enhancing organ transplants.
[1] euthanasia, organ donation, cDCD, deceased donation, transplantation
