Expansion of machine perfusion for liver transplantation in the United States demonstrates increased organ utilization and improved DCD graft survival
Steven Wisel1, Justin A Steggerda1, Michie Adjei1, Irene K Kim1.
1Comprehensive Transplant Center, Cedars-Sinai Medical Center, Los Angeles, CA, United States
Background: The United States is currently experiencing a paradigm shift in liver transplantation with rapid adoption of machine perfusion for liver transplantation. Despite multiple international trials identifying the efficacy of both hypothermic and normothermic machine perfusion, the current real-world use of machine perfusion (MP) technology in the United States is unknown. Given the dramatic surge in MP use within the United States, this study assesses national data to evaluate the impact of MP on organ utilization and transplant outcomes.
Methods: The OPTN Standard Transplant Analysis and Research database was used to identify all donor livers procured with the intent for transplant between 10/27/2015 (date of first recorded machine perfusion) and 6/30/2023 (n=67,795). Liver allografts were divided into donation after brain death (DBD, n=59,957) and donation after circulatory death (DCD, n=7,873) cohorts and evaluated by standard cold storage (SCS) or MP preservation method. Donor demographics, organ utilization, and graft survival were evaluated. Results were analyzed using Kruskal-Wallis and chi square testing, with graft and patient survival analyzed using Kaplan-Meier methods.
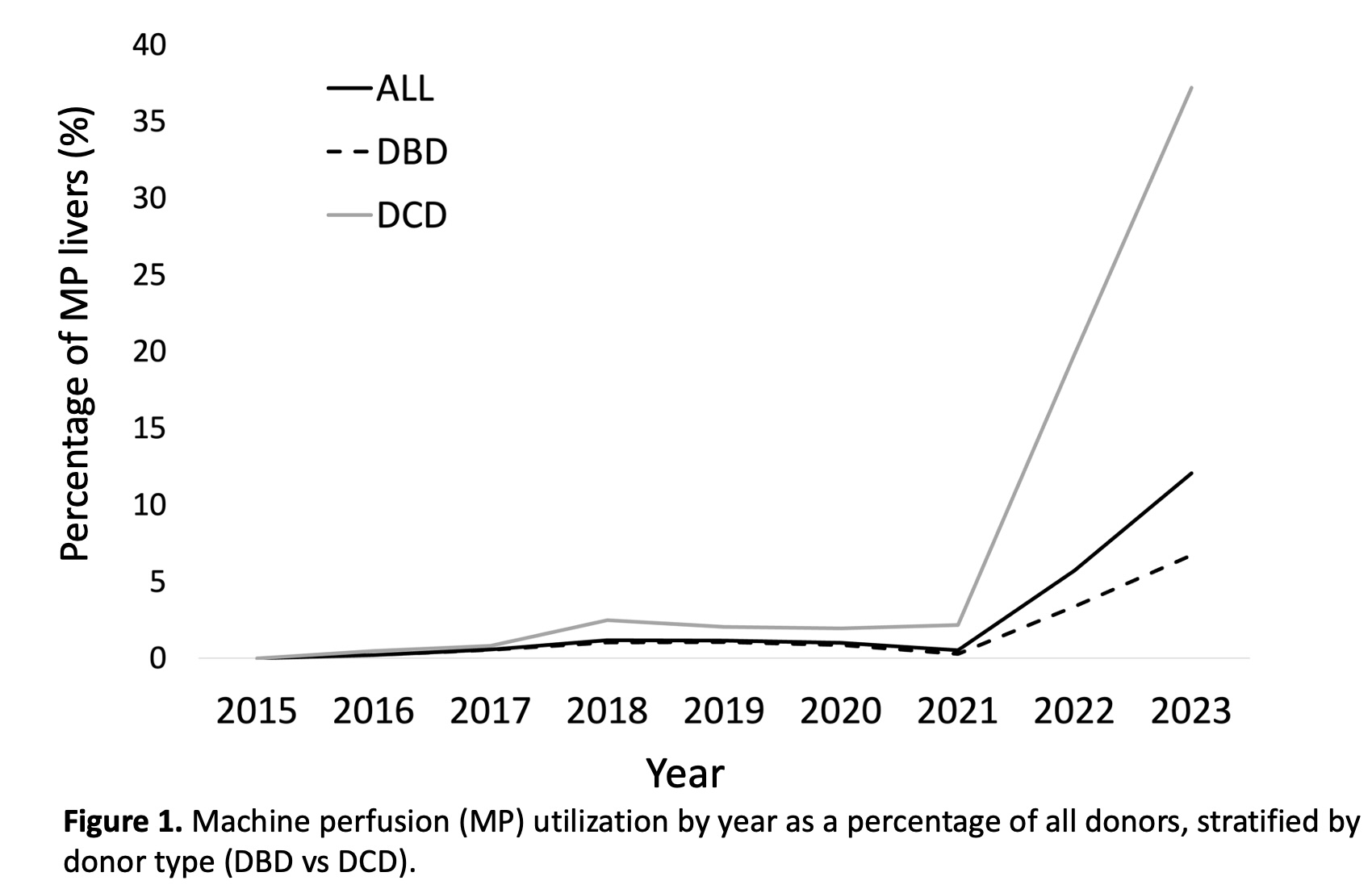
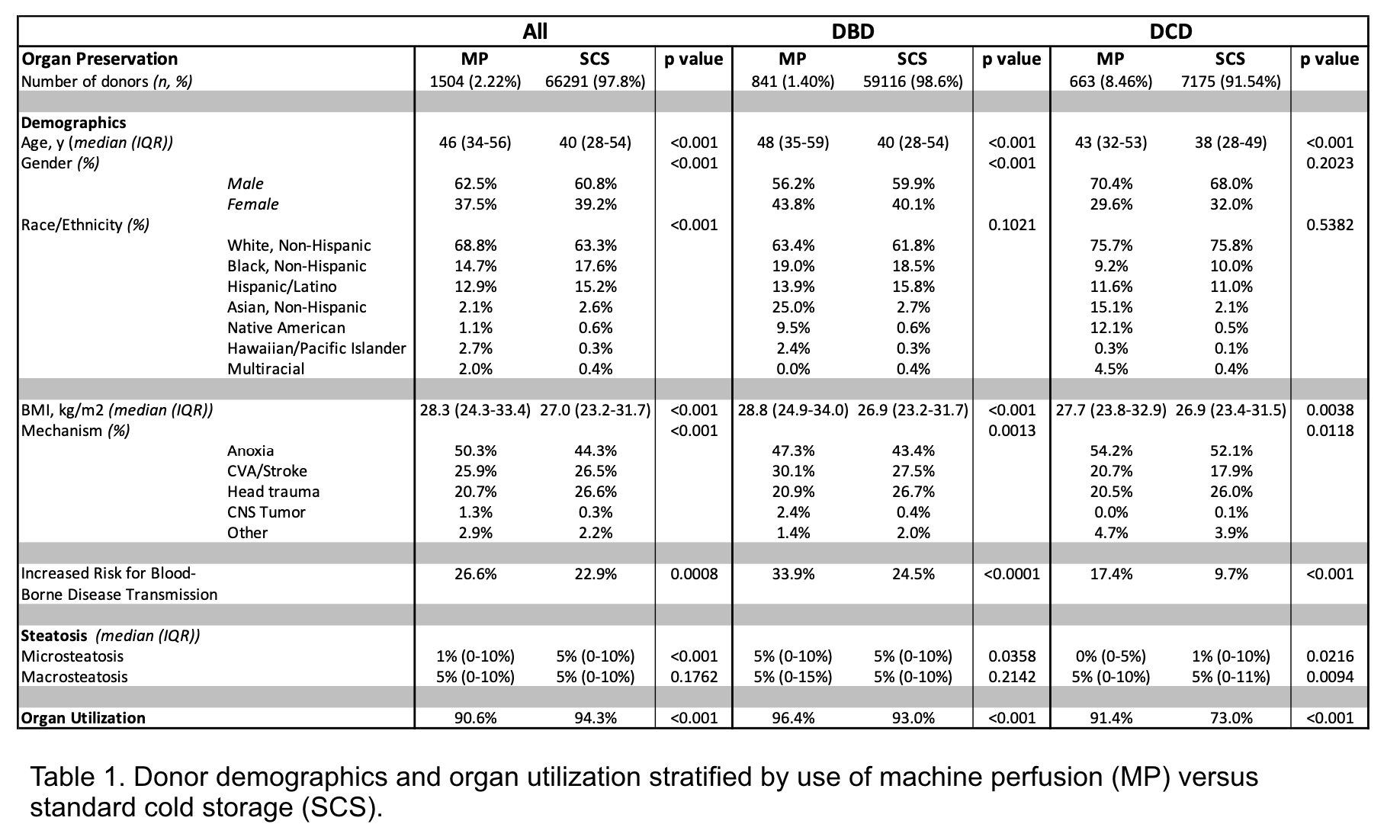
Results: Utilization of MP has increased since 2021, with 12.5% of all livers and 37.2% of DCD livers undergoing MP by 2023 (Figure 1). Normothermic MP was used for 82.6% of MP livers, while 6.7% underwent hypothermic perfusion, and 10.8% were other/unknown. Compared to donors of SCS livers, MP liver donors were older (median age 46 vs. 40 years), had higher BMI (28.3 vs. 27.0 kg/m2), and were more likely male (62.5% vs. 60.8%; p<0.001 for all, Table 1). When reported, donor livers had similar levels of macrosteatosis (median 5% for all groups). Graft utilization rate was higher for MP livers in both DBD (96.4% vs 93%, p<0.001) and DCD (91.4% vs 70.3%, p<0.001) compared to SCS livers. MP-preserved grafts had superior three-year graft survival for DCD liver transplants (p=0.037), while three-year graft survival was similar between MP and SCS livers from DBD donors (p=0.516). Patient survival was similar across all groups at 3 years (p=0.322).
Conclusions: This study confirms a dramatic increase in the use of MP technology for liver allograft preservation in the United States, with associated increased rates of liver utilization and improved graft survival compared to SCS methods for grafts from DCD donors. Further monitoring of MP outcomes is required to understand the long-term benefits.
[1] Organ preservation
[2] Machine perfusion
[3] Organ utilization
[4] Liver transplant
