Reconsidering the impacts of morbid obesity on kidney transplantation in the age of robotic-assisted kidney transplantation
Steven Wisel1, Justin A Steggerda1, Miguel Burch2, Edmund Huang1, Irene K Kim1.
1Comprehensive Transplant Center, Cedars-Sinai Medical Center, Los, CA, United States; 2Department of Surgery, Cedars-Sinai Medical Center, Los Angeles, CA, United States
Background: In the United States, morbid obesity continues to limit access to kidney transplant (KT) due to technical complexity and risk of surgical complication. Robotic-assisted kidney transplantation (RAKT) can overcome the technical challenges of KT in the obese population, but the impact of morbid obesity on KT outcomes must be considered to appropriately guide the rapid expansion of RAKT for obese recipients.
Methods: A retrospective analysis of the UNOS/OPTN database identified all KT recipients from 2005-2019. Transplant recipients were analyzed by donor type: deceased donor (n=138,132) versus living donor (n=68,957). Donor and recipient demographics were used to construct a multivariable regression model stratifying recipients into cohorts by BMI (<18.5kg/m2, 18.6-24.9kg/m2, 25-29.9kg/m2, 30-34.9kg/m2, 35-39.9kg/m2, ≥40kg/m2), with 70% of patients were included in the test cohort and 30% in the validation cohort. The primary outcome was 5-year graft survival, with secondary endpoints incidence of delayed graft function, post-transplant glomerular filtration rate (eGFR; CKD-EPI Creatinine Equation (2021)), and acute rejection episodes. Additionally, we evaluated all KT performed at our center during a 3-year period (2018-2021; n=806) to evaluate additional outcomes not available in the UNOS/OPTN database.
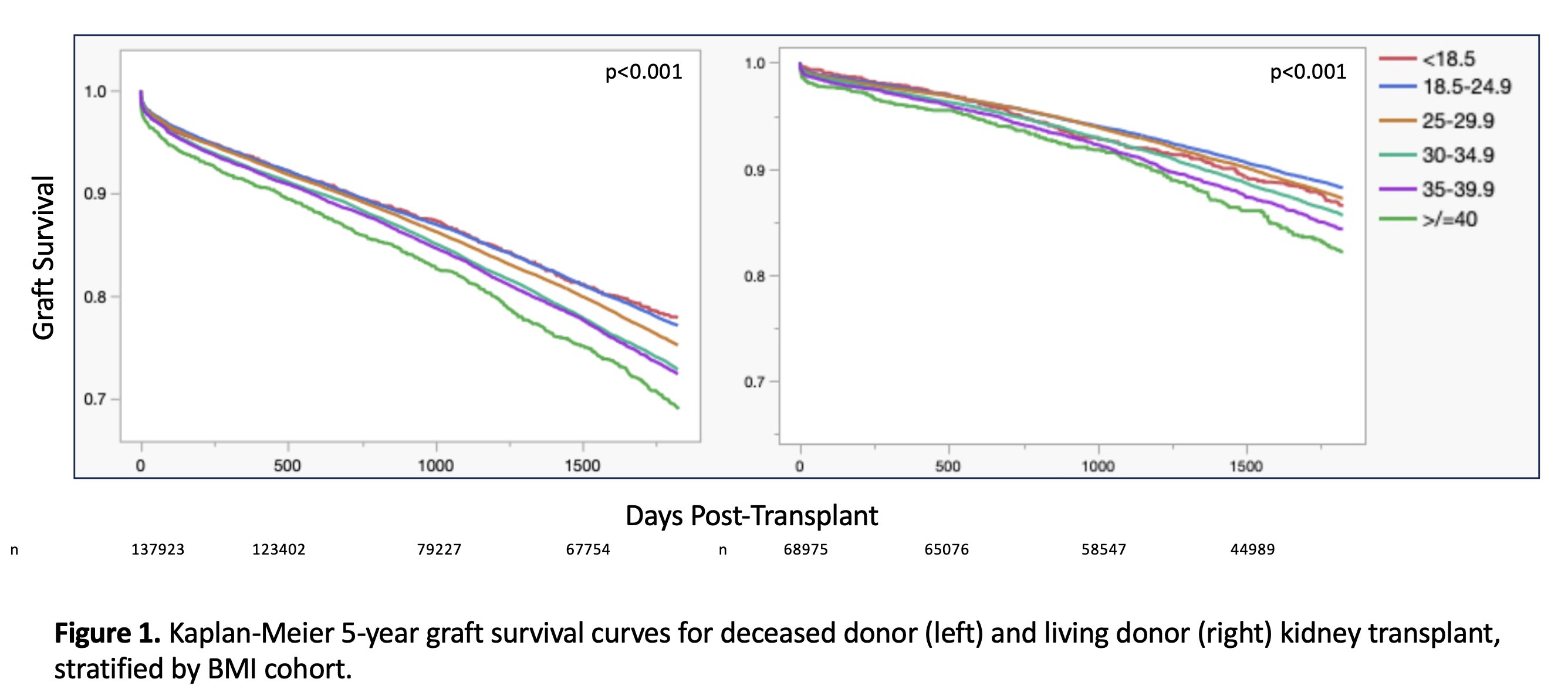
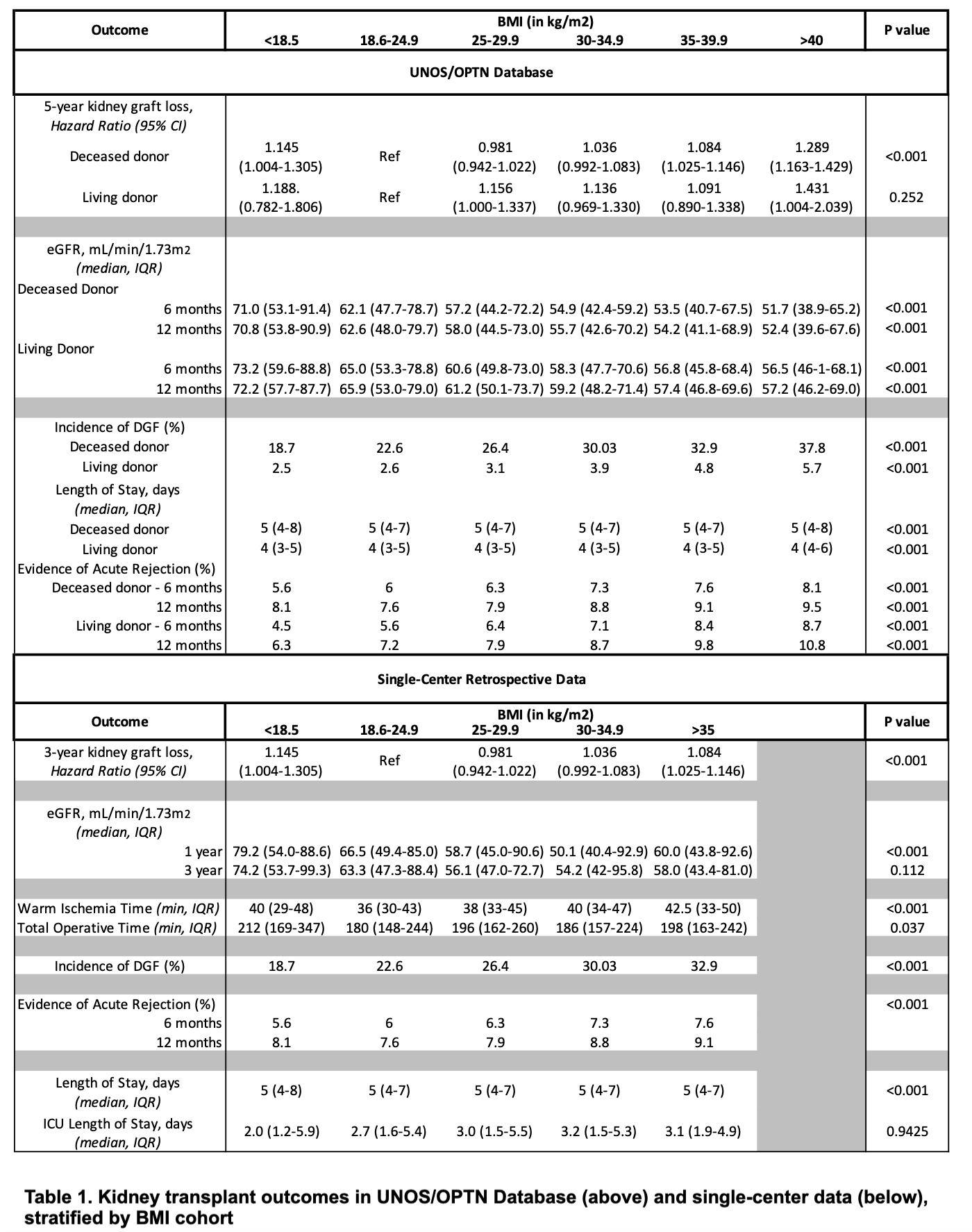
Results: In UNOS/OPTN data, elevated BMI correlated with inferior graft survival by Kaplan-Meier analysis for both living and deceased donor KT (p<0.001 for both; Figure 1). Multivariable analysis revealed elevated BMI was associated with inferior 5-year graft survival in deceased donor KT, with morbidly obese patients (BMI≥40kg/m2) at the highest risk for graft loss (HR = 1.289, 95% CI 1.163-1.429; Table 1). Higher BMI correlated with inferior graft function by eGFR at 6 and 12 months for both living and deceased donor recipients (p<0.001 for all, Table 1). Furthermore, elevated BMI corresponded to increased incidence of delayed graft function, and increased risk for acute rejection episodes at 6 and 12 months (p<0.001 for all; Table 1). While statistically significant, there was a modest increase in length of stay for patients with BMI ≥40kg/m2 and BMI <18.5kg/m2. In single-center analysis, increasing BMI was associated with prolonged warm ischemia time (p<0.001) and total operative time (p=0.037)
Conclusions: Morbid obesity impairs KT outcomes. RAKT eases the technical barriers associated with transplantation, potentially expanding access to life-saving KT for obese patients. Expansion of BMI criteria for KT will increase organ access, but should be combined with a weight loss algorithm incorporating medical and surgical weight loss strategies to ensure successful long-term graft outcomes.
[1] kidney transplant
[2] recipient selection
[3] Obesity and weight loss
[4] Graft outcomes
