The association of hepatic artery resistive index and graft failure; Analysis of various cut-off values
Rozita Khodashahi1,2,3, Amir Mahmoud Ahmadzadeh1,4, Mohsen Aliakbarian1,5, Hoda Rahimi1,6, Aref Abdollahzade1,6.
1Transplant Research Center, Clinical Research Institute, Mashhad University of Medical Sciences, Mashhad, Iran; 2Clinical Research Development Unit, Imam Reza Hospital, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran; 3Department of Infectious Diseases and Tropical Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran; 4Department of Radiology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran; 5Surgical Oncology Research Center, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran; 6Targeted Drug Delivery Research Center, Pharmaceutical Technology Institute, Mashhad University of Medical Sciences, Mashhad, Iran
Introduction: Hepatic artery resistive index (HARI), is a parameter measured based on the factors obtained from Doppler ultrasonography (DUS). Herein, we aimed to evaluate the predictive values of HARIs assessed on different days in assessing liver graft failure (GF) at 1-month, 3-month, and 12-month time points. We also investigated the time-to-event probabilities between two groups according to the various HARI cut-offs. The day-by-day correlations between HARI values and liver function markers were assessed as well.
Method: All the patients that received deceased donor LT between January 10th 2014 and September 11th 2022 and were followed up for at least 12 months were assessed for potential inclusion. Patient information, including DUS data and the levels of liver function markers were collected. GF at 1-month, 3-month, and 12-month time points were also assessed. GF was defined as death or retransplantation, whichever occurs earlier. DUS examination was performed on a daily basis in the 96 hours after LT surgery and the HARI was calculated. Spearman correlation test and receiver operating characteristic (ROC) curve analysis was performed. We also used the semiparametric proportional hazards Cox model to quantify the association between the time-to-event and HARI with various cut-off values at different days. Kaplan-Meier curves were then drawn for significant results.
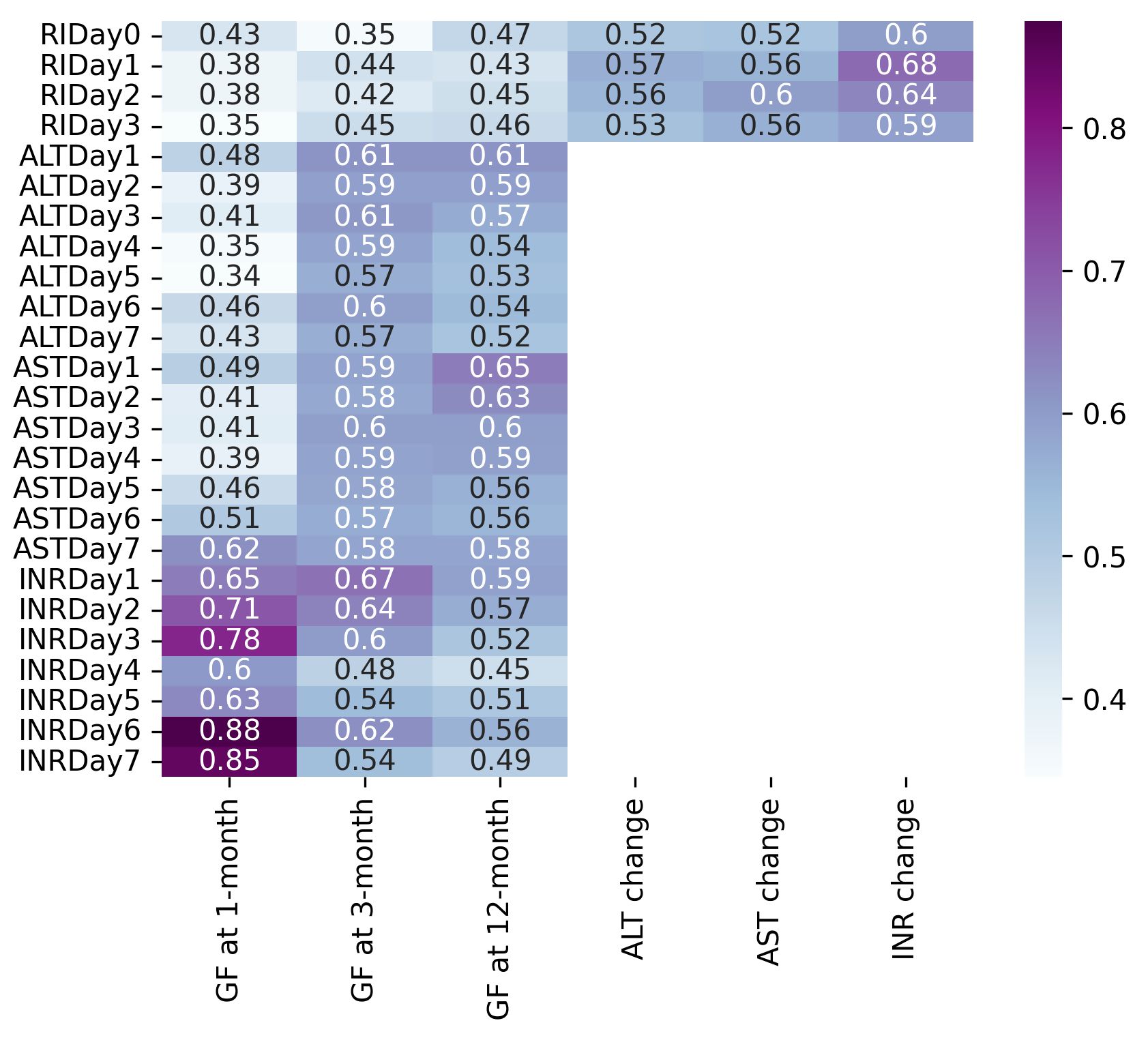
Results: 323 patients (216 M/107 F, median age: 52 [37-60]) were included in this study. There were significant negative correlations between all daily HARI values and ALT measurements. However, all the correlations were weak or moderate (r < 0.3 for all). For AST, no significant correlation was found between RIDay0 and ASTDay4, ASTDay5, and ASTDay7, RIDay1 and ASTDay7, as well as RIDay2 and ASTDay7. Other correlations were weakly or moderately significant (r < 0.4 for all). Regarding INR, there was a significant negative correlation only between RIDay1 and INRDay1 which was weak (p = 0.023, r = (-0.127)). All of the measured HARIs had low AUC for predicting GF (AUC < 0.5 for all). The AUCs of HARI values for predicting liver markers changes ranged between 0.52 to 0.57 for ALT, 0.52 to 0.60 for AST, and 0.60 to 0.68 for INR (Figure 1).
Patients with RIDay1 within 0.50-0.80 range had a 2-fold probability of GF compared to the patients with RIDay1 < 0.50 or RIDay1 > 0.80 (HR = 2.01 [1.03-3.91], p = 0.04). Also, the probability of GF was 2.5-fold in the patients with RIDay3 ≤ 0.70 and in patients with RIDay3 within (0.50-0.70), (0.55-0.70), and (0.60-0.70) ranges (Figure 2).
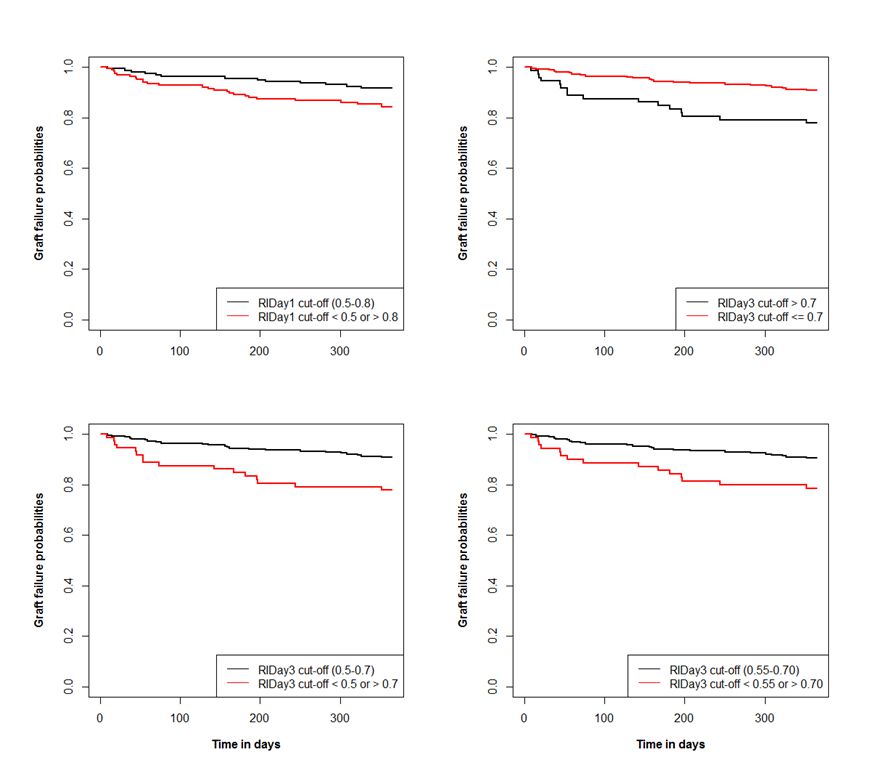
Conclusion: The correlations between HARI values and liver markers were weak to moderate. The HARIs did not yield high predictive values neither for GF nor for liver marker changes. Patients with RIDay1 within the 0.50-0.80 range and RIDay3 ≤ 0.70 or within (0.50-0.70), (0.55-0.70), and (0.60-0.70) ranges had higher probabilities of GF.
We would like to thank the Transplant Research Center, Mashhad University of Medical Sciences, for providing supports in this manuscript. We would also like to thank the Clinical Research Development Unit, Imam Reza Hospital, Mashhad University of Medical Sciences, for their assistance in this manuscript.
[1] Resistive index
[2] Graft failure
[3] Doppler ultrasonography
[4] Ultrasound
[5] Survival analysis
