Vibration-controlled transient elastography as a non-invasive tool to exclude hepatic steatosis in living liver donor evaluation
Sarita Ratana-Amornpin1,2, Pongphob Intaraprason1,2, Nuttapon Arpornsujaritkun2,3, Goragoch Gespresert2,3, Bundit Sakulchairungrueng2,3, Sutipong Jongjirasiri2,4, Pattana Sornmayura2,5, Piyaporn Kaewduang1,2, Sasiwimol Thurapokol1, Abhasnee Sobhonslidsuk1,2.
1Division of Gastroenterology and Hepatology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 2Excellence Center for Organ Transplantation, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 3Vascular and Transplantation Unit, Department of Surgery, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 4Department of Diagnostic and Therapeutic Radiology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 5Department of Pathology, Faculty of Medicine, Ramathibodi Hospital, Bangkok, Thailand
Background: The number of living donor liver transplantations (LDLT) has been increasing because of the shortage of deceased donors. LDLT with hepatic steatosis > 20 – 30% is a risk factor for post-transplant liver graft dysfunction. Vibration-controlled transient elastography (VCTE) with a controlled attenuation parameter (CAP) is a non-invasive test used to assess hepatic steatosis. Using VCTE with CAP as an assessment of hepatic steatosis for living-donor evaluation might eliminate the need for invasive liver biopsies. This study aimed to evaluate the correlation between CAP and histologic amount and percentage of liver fat and between CAP and magnetic resonance imaging fat signal fraction (MRI-FSF).
Materials and methods: This was a retrospective study of living donors for LDLT between January 2019 and June 2023 in Ramathibodi Hospital, Bangkok, Thailand. Subjects with pre-existing liver disease, including hepatitis B virus infection, hepatitis C virus infection, or alcoholic liver disease, were excluded. Stepwise living donor evaluations included a medical history review, physical examination, laboratory, imaging studies, VCTE, MRI-FSF, and liver biopsy (only for indicated subjects). Histopathological reports were obtained during the pre-LDLT evaluation or surgery. We defined hepatic steatosis ≥5% as the cut-off level because it was intended to be a screening tool for liver donor evaluation. Receiver operating characteristic (ROC) curve analysis was used to predict hepatic steatosis with appropriate sensitivity, specificity, and Youden’s index for liver donor screening.
Results: Fifty-three subjects were living donors, including 15 (28.3%) men with a mean age of 31.9 ± 6.9 years. Body mass index, CAP, alanine transaminase, and fasting blood sugar levels were significantly higher in subjects with hepatic steatosis ≥5% than in those with hepatic steatosis <5%. The area under the curve (AUC) for CAP in predicting hepatic steatosis ≥5% by histology was 0.851 (95% CI 0.727–0.974, p < 0.001). The optimal cutoff value of CAP was ≥240 dB/m to detect histological steatosis ≥5%, with a sensitivity of 72.7% and a specificity of 83.3%. To predict hepatic steatosis >5% using MRI-FSF, the AUC for CAP was 0.771 (95% CI, 0.609–0.933; p = 0.004). The optimal cut-off value of CAP was ≥254 dB/m for the detection of MRI-FSF >5%, with a sensitivity of 61.5% and a specificity of 92.1%.
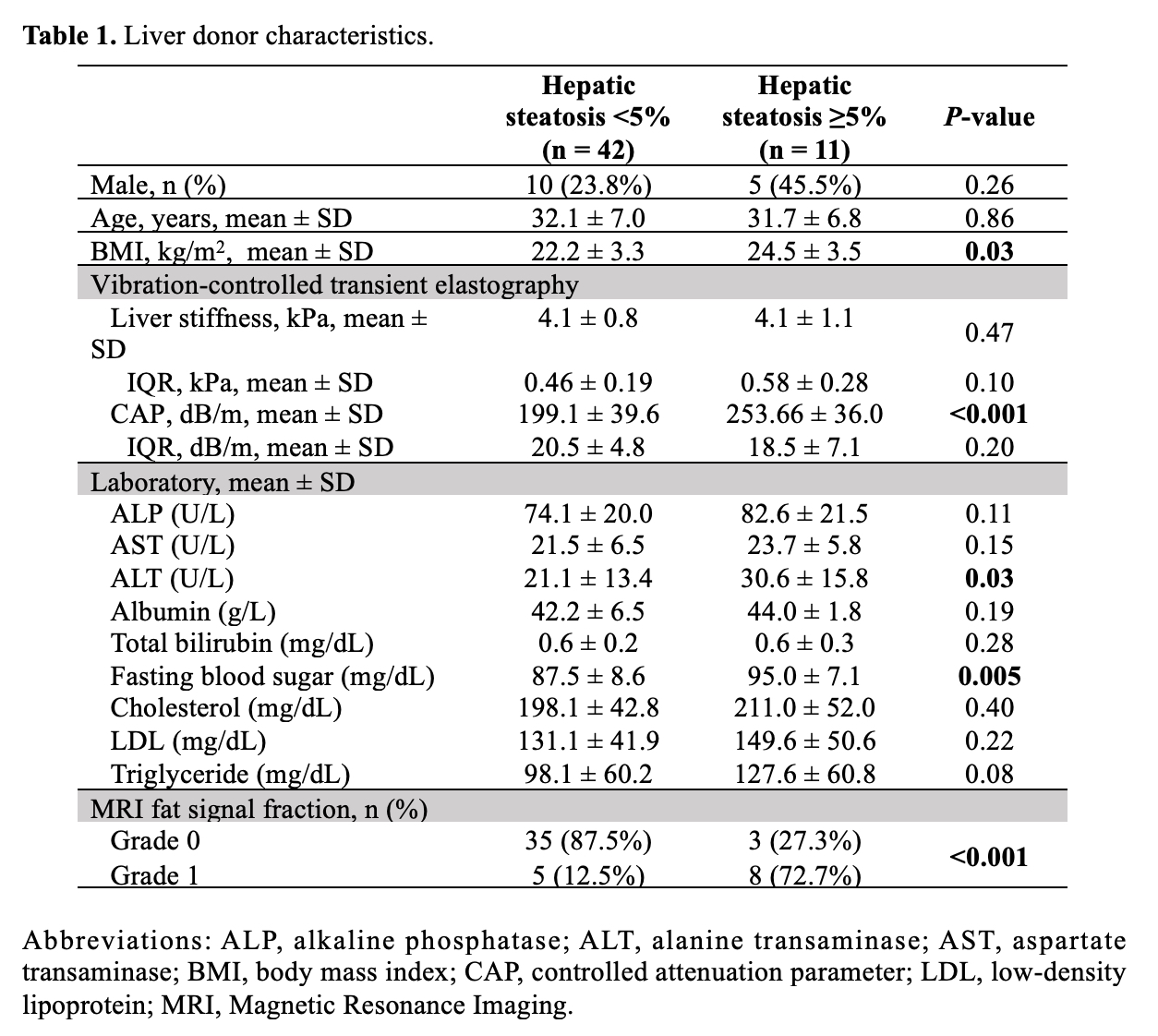
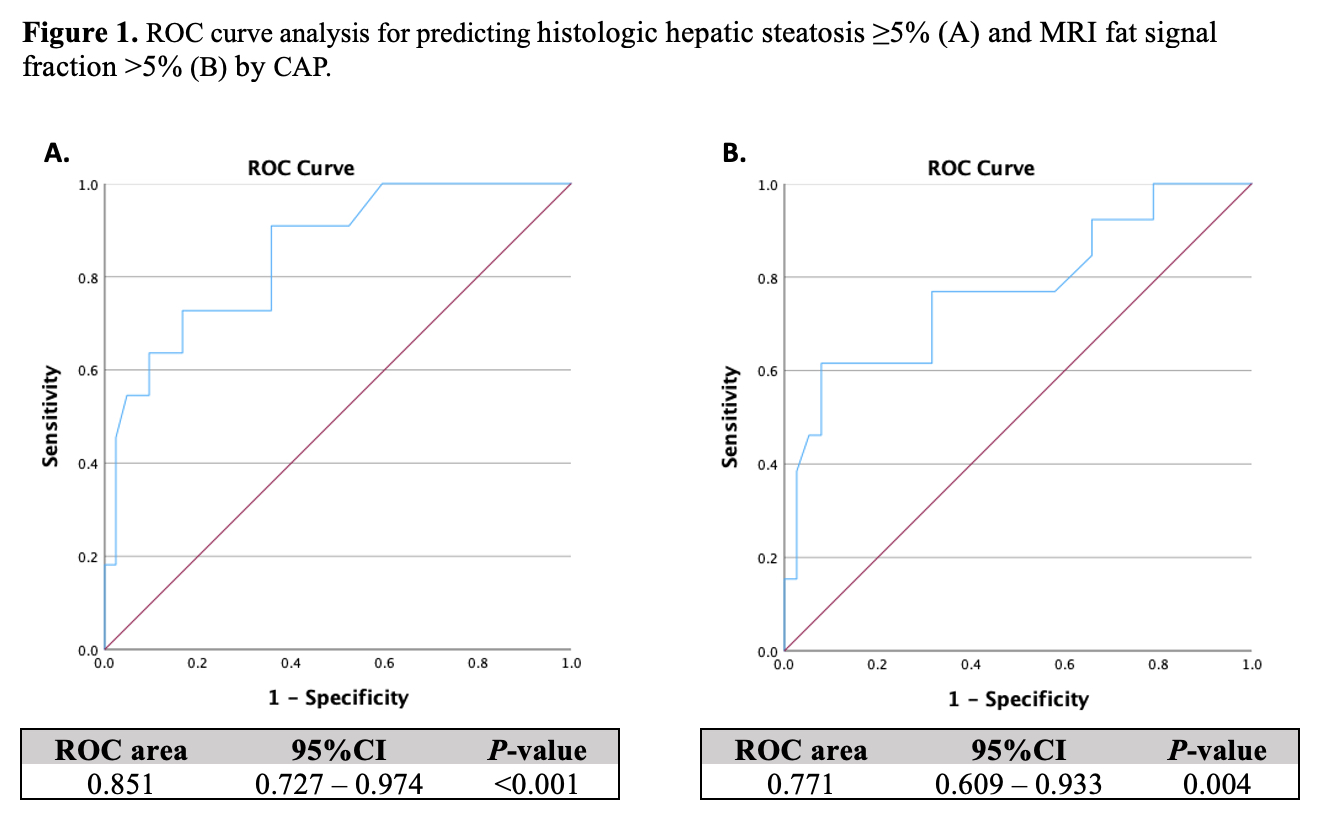
Conclusions: VCTE is a noninvasive test that can be used for hepatic steatosis assessment in living donors for LDLT evaluation. Subjects evaluated for living donors with CAP <240 dB/m avoided liver biopsy. Further studies are needed to confirm the results of this study.
