Vacuum-assisted laparostomy for delayed abdominal closure in pediatric liver transplantation: A case series
Yusra Safarova1, Sergei Meshcheriakov1, Artem Monakhov1,2, Olga M. Tsirulnikova1,2, Ekaterina Shadrina1, Irina Pashkova1,2, Ekaterina Ryzhik1, Nidzhat Yusuf1, Sergei V. Gautier1,2.
1Liver Transplantation Department, V.I. Shumakov Transplantology & Artificial Organs National Medical Research Center, Moscow, Russian Federation; 2Chair of transplantation and artificial organs, Sechenov University, Moscow, Russian Federation
Introduction: Liver transplantation is often the only treatment option for end-stage liver diseases in pediatric patients. The mismatch in size between the recipient's abdominal cavity and an oversized liver graft can lead to the development of large-for-size syndrome (LFSS). However, the shortage of appropriately sized donor organs for pediatric patients necessitates the use of larger grafts, which may be disproportionated to the recipient's abdominal cavity. Factors associated with LFSS, including diaphragmatic excursion restriction, visceral perfusion impairment, and graft compression in the abdominal cavity, can affect graft function and recipient morbidity.
Methods: We present a series of 7 pediatric cases operated between December 2022 and March 2024 at the single center. These cases involved liver transplantation using the left lateral section (LLS). Delayed closure of the abdominal cavity through vacuum-assisted laparostomy was applied to avoid the LFSS. The indications for laparostomy were based on the graft-to-recipient weight ratio (GRWR), the CT-calculated thickness disparity between LLS and the recipients's abdominal cavity, and worsening parameters of artificial ventilation during test abdominal wall approximation. We favored this approach to abdominal closure to prevent the abdominal compartment syndrome.
Results: The median age of the patients was six months (range: 3-8 months), and the median body weight was 6.7 kg (range: 4.3-7.3 kg). The median PELD score was 23, and the median GRWR was 4.6% (ranging from 3.6% to 7.1%). Final closure of the abdominal cavity was performed at 7 to 24 postoperative days, and took 1 to 3 procedures of stepwise closure of the abdominal wall defect using native tissues. No surgical complications, including biliary and vascular, or complications associated with using this approach occurred. No surgical complications occurred, including biliary and vascular, nor any complications associated with this approach.
Conclusion: This case series demonstrates the safety and advantages of vacuum-assisted laparostomy for delayed closure of the abdominal cavity in a selective group of patients after pediatric liver transplantation. This approach can be an effective alternative to anatomical or non-anatomical reduction of the liver graft, as well as the use of a Bogota bag or abdominoplasty using synthetic materials (ePTFE, GoreTex). Vacuum-assisted laparostomy protects the integrity of the abdominal wall and minimizes the risk of infection.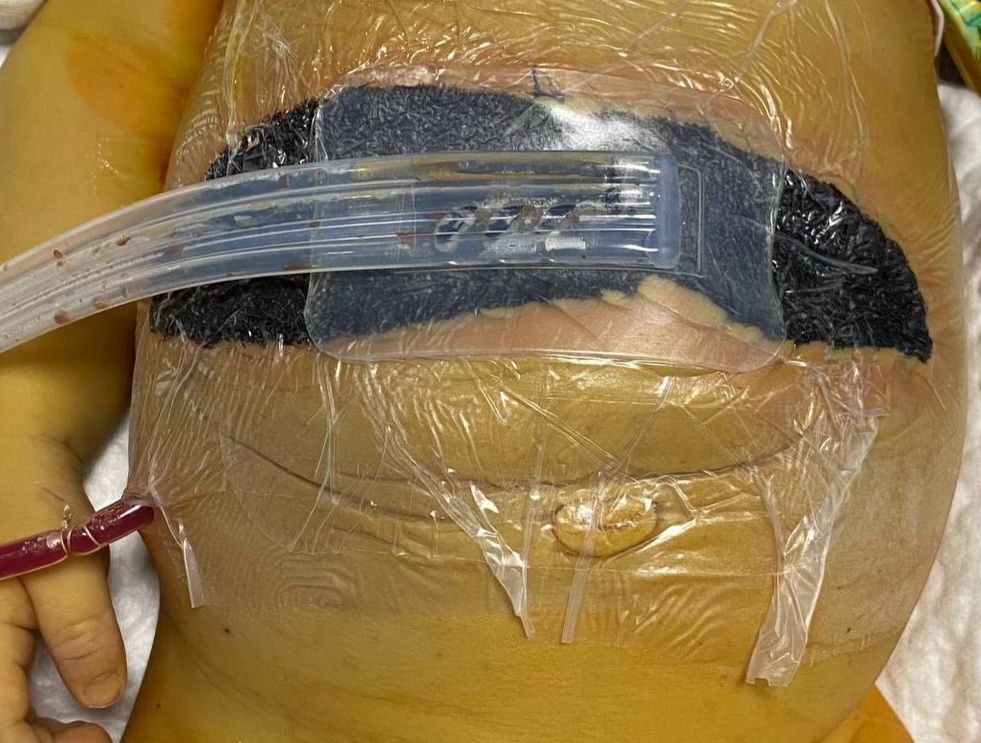
[1] living donor liver transplantation
[2] large-for-size syndrome
[3] delayed abdominal closure
[4] pediatric transplantation
