A novel antibody-mediated rejection model for mouse intestinal transplantation and its histopathological characteristics
Takuro Fujita1, Hajime Matsushima1, Taichiro Kosaka1, Akihiko Soyama1, Takanobu Hara1, Tomohiko Adachi1, Susumu Eguchi1.
1Department of Surgery, Graduate School of Biomedical Sciences Nagasaki University , Nagasaki, Japan
Background: Intestinal transplantation is the ultimate treatment option for short bowel syndrome and irreversible intestinal failure. Despite significant advances in immunosuppression therapy, peritransplant management, and surgical technique during the past few decades, long-term outcomes remain considerably lower than those for other organ transplantations. It has been reported that the presence of preformed DSAs and the formation of de novo DSAs posttransplant are closely associated with increased risk of graft loss due to hyperacute and chronic rejection via antibody-mediated rejection (AMR) in intestinal transplantation. However, its pathogenesis and histopathological characteristics for diagnosis remain unclear. The availability of animal models mimicking human AMR is essential to understand its pathogenesis and develop new treatment strategies. We performed intestine transplantation in presensitized mice with donor skin grafts for the first time and evaluated the histopathology of intestinal grafts.
Methods:Full-thickness skin grafts from donor B6 mice was grafted onto the back of recipient C3H mice, and circulating DSAs at days 3, 7, and 14 were evaluated using mean fluorescence intensity (MFI) by flow cytometry. Intestinal grafts from B6 mice were transplanted in presensitized mice at day 14 after skin transplantation.
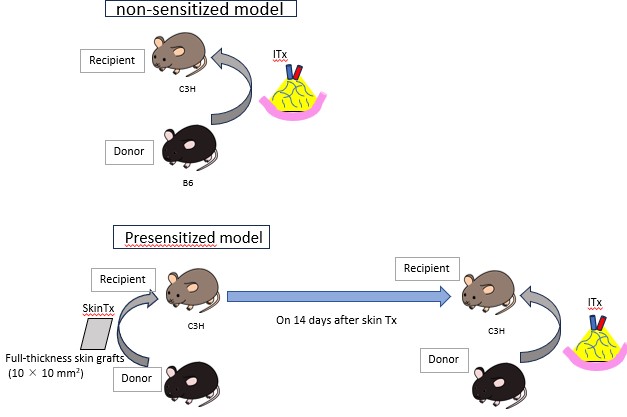
Intestinal grafts were evaluated on days 2 and 4 after intestine transplantation. The nonpresensitized mice recipients were evaluated as a control, and histopathological findings were compared.
Results: The presensitized recipients (n=6) and nonpresensitized recipients (n=6) were compared. The MFI of circulating DSAs increased over time in the presensitized recipients. Intestinal grafts were rejected more severely in the presensitized recipients at both day 2 and day 4.Also the villous heights on day 2 were significantly shorter in the presensitized recipients than non-sensitized recipients (P =0.01).Immunostaining showed no significant difference in the number of infiltrating CD4- and CD8-positive cells between the groups. On the other hand, the number of infiltrating CD20- and CD68-positive cells was significantly higher in the presensitized recipients on day 2 (CD20: P =0.04, CD68: P <0.01). In the presensitized recipients, C3 and C4 depositions were observed on vascular endothelium of intestinal grafts at day 2 after transplantation.
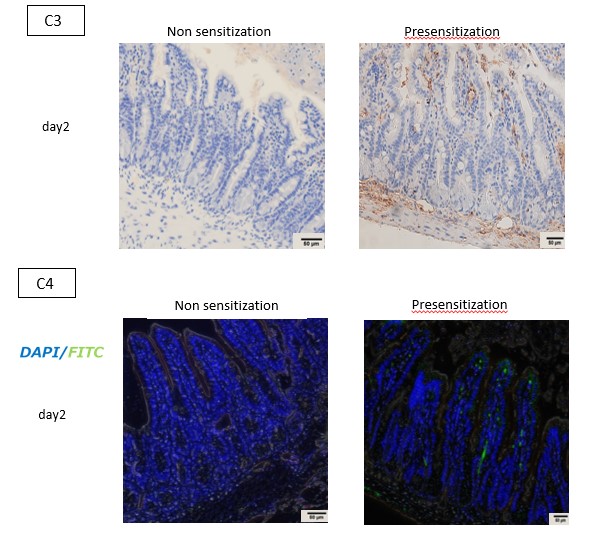
Conclusion: A presensitized mouse model of intestinal transplantation was successfully established. Our animal model might be a powerful tool to understand the pathogenesis of AMR and explore the effective treatment strategies. Furthermore, as with other solid organs transplantation, early detection of C3 and C4 depositions might be helpful for diagnosing AMR in intestinal transplantation.
[1] intestinal transplantation, presensitization, donor-specific antibody, antibody-mediated rejection
