Torque teno virus for predicting severe infections and biopsy-proven rejection in prevalent kidney transplant recipients: An inter-rim analysis of a single-centre prospective cohort study
Ian Tatt Liew1, Quan Yao Ho1, Deborah Chooi Mun Lai2, Rou Wei Lim3, Puay Hoon Lee3, Kun Lee Lim2, Carolyn Shan-yeu Tien1, Sobhana Thangaraju1, Lynette Lin Ean Oon2, Terence Kee1.
1Renal Medicine, Singapore General Hospital, Singapore, Singapore; 2Molecular Pathology, Singapore General Hospital, Singapore, Singapore; 3Pharmacy, Singapore General Hospital, Singapore, Singapore
Introduction: Torque teno virus (TTV) is a promising biomarker for immune monitoring amongst solid organ transplant recipients and may be used to predict both infections and rejection. However, its role in kidney transplant recipients (KTRs) on stable immunosuppression beyond 1 year after transplantation is less well-established.
Method: This is a planned inter-rim analysis of a single-centre prospective cohort study. KTRs who are on stable immunosuppression for at least 3 months and had been followed up for at least 90 days were included. Baseline TTV viral loads were collected upon recruitment, along with clinical data and other potential biomarkers. The primary outcome was severe infections defined as infections requiring hospitalization and secondary outcomes included biopsy-proven rejection (BPAR). Subjects were followed-up until there was a change of immunosuppression.
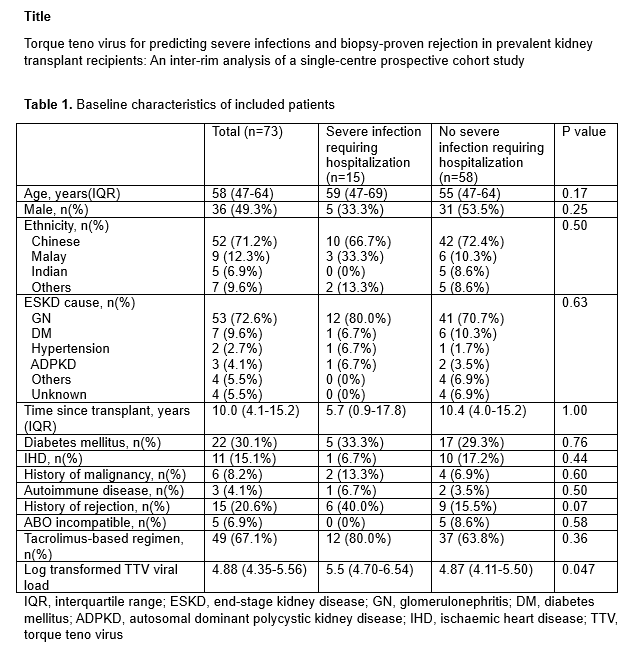
Results: A total of 73 patients with a median transplant vintage of 10.0 (interquartile range (IQR) 4.1-15.2) years and median follow-up duration of 154 (IQR 130-184) days were included (Table 1), of which 15 (20.6%) developed severe infections requiring hospitalization. While patients with severe infections had higher log transformed TTV viral loads (log TTV) (5.50 vs 4.87 copies/ml, p=0.047), log TTV was not associated with severe infections (odds ratio (OR) 1.26, 95% confidence interval (CI) 0.84-1.89, p=0.27) with an area under receiver operating curve (AUROC) of 0.64.
17 patients underwent kidney allograft biopsy, of which 9 (52.9%) demonstrated BPAR. Patients with BPAR had lower log TTV compared to those without BPAR (4.90 copies/ml vs 6.44 copies/ml, p=0.02). The association of log TTV with BPAR trended towards statistical significance (OR 0.34, 95% CI 0.12-1.03, p=0.056), with an AUROC of 0.79. All patients with log TTV of <4.53 were diagnosed with BPAR while, all with >6.23 had no rejection.
On multivariable analysis, higher log TTV was associated with diabetes mellitus as a cause of ESKD (coefficient 0.90, 95% CI 0.11-1.69, p=0.03), tacrolimus use (coefficient 0.84, 95% CI 0.35-1.33, p=0.001) and lower CD56 levels (-0.002, 95% CI -0.003 to -0.0002, p=0.02).
Conclusion: For KTRs on stable immunosuppression for at least 3 months, log TTV levels were higher in patients who developed infections requiring hospitalization. For KTRs undergoing kidney allograft biopsy, pre-biopsy log TTV levels may predict BPAR. TTV viral loads were associated with clinical and laboratory factors related to degree of immunosuppression.