International graft preservation practices and anastomosis time impacting delayed graft function in kidney transplantation
Bridget C. Vaughan1, Thomas A. Sorrentino1, Jonathan E. Freise1, Victoria Wu2, Marc L. Melcher2, James M. Gardner1, Keith S. Hansen1.
1University of California, San Francisco, San Francisco, CA, United States; 2Stanford Medicine, Stanford, CA, United States
Introduction: Efforts to reduce delayed graft function (DGF) in kidney transplant include a variety of graft preservation techniques not yet standardized across centers. Graft preservation via warm ischemic time (WIT) reduction has primarily been addressed in the perioperative setting via increasing adoption of machine perfusion. Additionally relevant WIT occurs intraoperatively and is captured by anastomosis time (AT) as a proxy. There is an existing gap in data following the cessation of AT collection by the Scientific Registry of Transplant Recipients (SRTR) in 2015. This study investigates graft preservation techniques and factors influencing AT in kidney transplantation across multiple centers, with a focus on their impact on DGF.
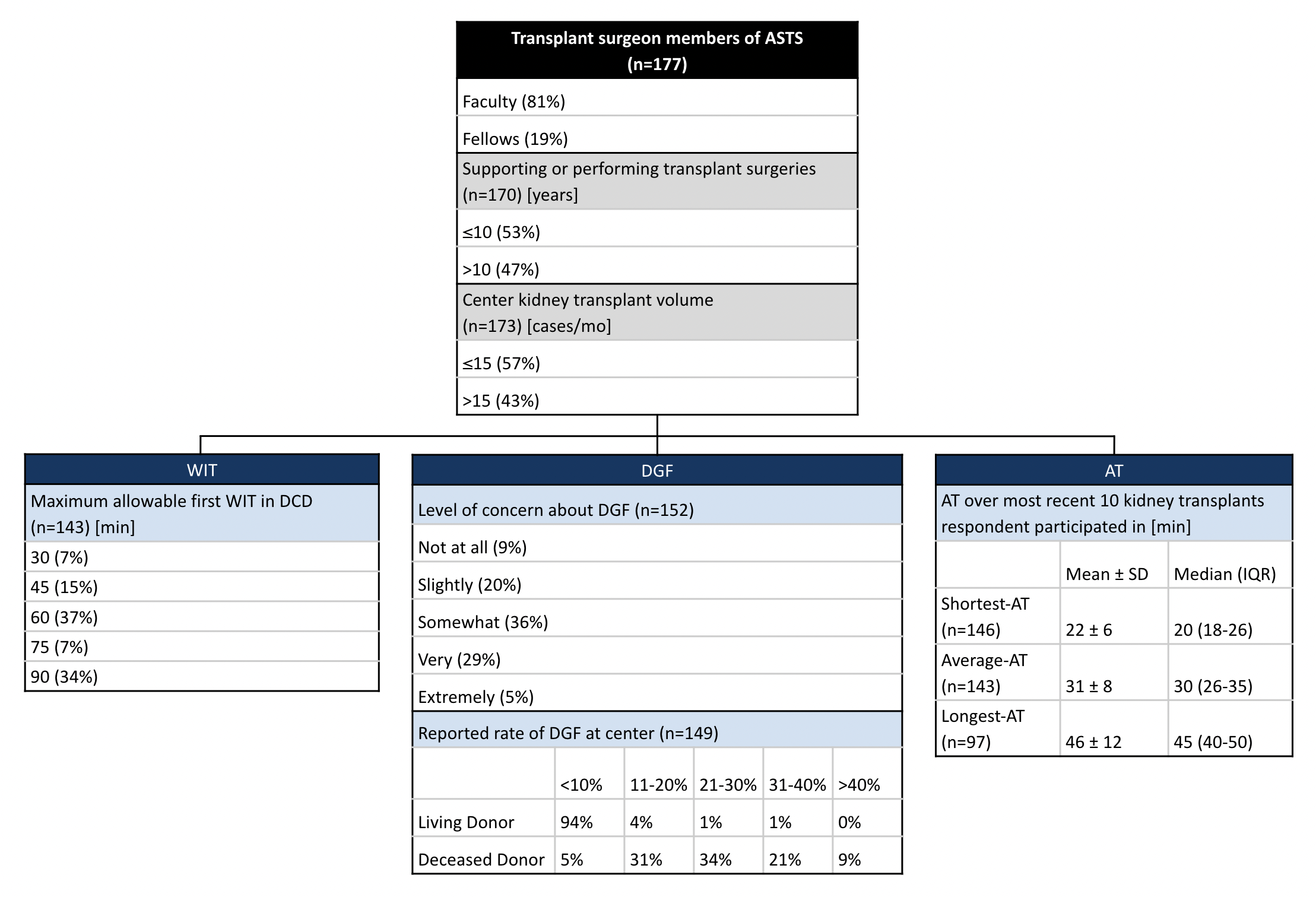
Methods: An online survey was conducted among 177 members of the American Society of Transplant Surgeons (ASTS) in 2021, with a response rate of 15.4% (177/1143). The survey addressed perceptions and practices of kidney allograft preservation, first WIT allowance in donation after circulatory death (DCD), DGF rates, and strategies to mitigate DGF.
Results: Respondents (n=177) represented programs across 19 countries. The majority of respondents would accept a maximum first WIT for DCD kidneys of 60 minutes (35%) or 90 minutes (32%). Surgeon-reported DGF rates were <10% (94%) for living donor grafts, and an average of 24.1% for deceased donor grafts. The majority reported concern about DGF (91%), with most surgeons (79%) taking multiple measures to reduce DGF, including machine perfusion (63%), minimizing cold (51%) and warm (33%) ischemic time, patient and organ selection (12%), optimizing immunosuppression (10%), and improving medical management of organ perfusion (9%). Considering their most recent ten kidney transplant cases, surgeons reported a shortest-AT of 22±6 minutes, longest-AT of 46±12 minutes, and average-AT of 31±8 minutes (mean ± SD). Factors contributing to shortest AT included favorable recipient anatomy (83%), more skilled or experienced surgical team (45%), favorable donor organ (23%), and patient factors (4%). Conversely, factors contributing to longest AT included unfavorable recipient anatomy (80%), unfavorable donor organ (48%), less skilled or experienced surgical team (18%), and re-anastomosis or repair (6%).
Conclusion: The survey highlights diverse practices in graft preservation and varying ATs across centers. There is a discrepancy between surgeons' estimations and SRTR data regarding deceased donor DGF rates and average AT. While surgeons accurately estimated living donor DGF rates, they underestimated deceased donor DGF rates (24.1% vs 28% [SRTR]) and median AT (30 min vs 38 min [SRTR]). Given the reported primary determinants of AT - anatomy and surgical expertise - are not easily modifiable, alternative approaches toward reducing WIT and enhancing organ preservation, such as improved graft temperature management, warrant further exploration.
[1] Kidney Transplantation
[2] Kidney
[3] Graft Preservation
[4] Delayed Graft Function
[5] Anastomosis Time
[6] Allograft Preservation
[7] Renal
[8] Transplantation
[9] Transplant Surgery
[10] Surgery
