Advancing living donor kidney transplantation: A comprehensive analysis of graft outcomes in single vs. Multiple renal arteries from over 2200 pure-laparoscopic living donor kidney transplantations
Devprakash Choudhary1, Shiva Kumar SP1, Bharat Bamaniya1, Karthik NVKN1, Parul Gupta3, Jasmine Sethi2, Sarbpreet Singh1, Deepesh Kenwar1, Ashish Sharma1.
1Department of Renal Transplant Surgery , PGIMER , Chandigarh, India; 2Department of Nephrology , PGIMER , Chandigarh, India; 3Department of Hospital Administration , PGIMER , Chandigarh, India
Introduction-Laparoscopic living-donor nephrectomy has become the standard of care in transplant centers performing living-donor kidney transplantation(LD-KT). Allografts with multiple renal arteries(MRAs) have been associated with higher incidences of vascular complications and poor graft-survival, leading to a cautious approach in selecting allografts with MRAs. Conflicting results from recent meta-analyses comparing graft-outcomes between single renal artery(SRA) and MRA have left the critical question unresolved: do the technical challenges faced by transplant surgeons during laparoscopic retrieval of MRA and surgical complexities during LD-KT translate into clinically significant differences in graft outcomes compared to SRA allograft? This study represents the largest single-center analysis examining the impact of MRA versus SRA on graft outcomes and death-censored graft and patient survival in pure-laparoscopic LD-KT.
Methods-This retrospective single-center study included LD-KT performed between September-2008 and December-2022. During this period, 2,780-KT were performed, 523-KT from deceased donors were excluded. The protocol for pure-laparoscopic LD-KT at the study center involved the laparoscopic procurement of kidneys with SRA or the left kidney in instances of MRAs. Donors and Kidney transplant recipients(KTRs) parameters were sourced from the department's prospectively maintained electronic-databases. KTRs with MRA and SRA grafts were compared across preoperative, intraoperative, and postoperative parameters. 9-KTRs were excluded from the analysis due to insufficient details.
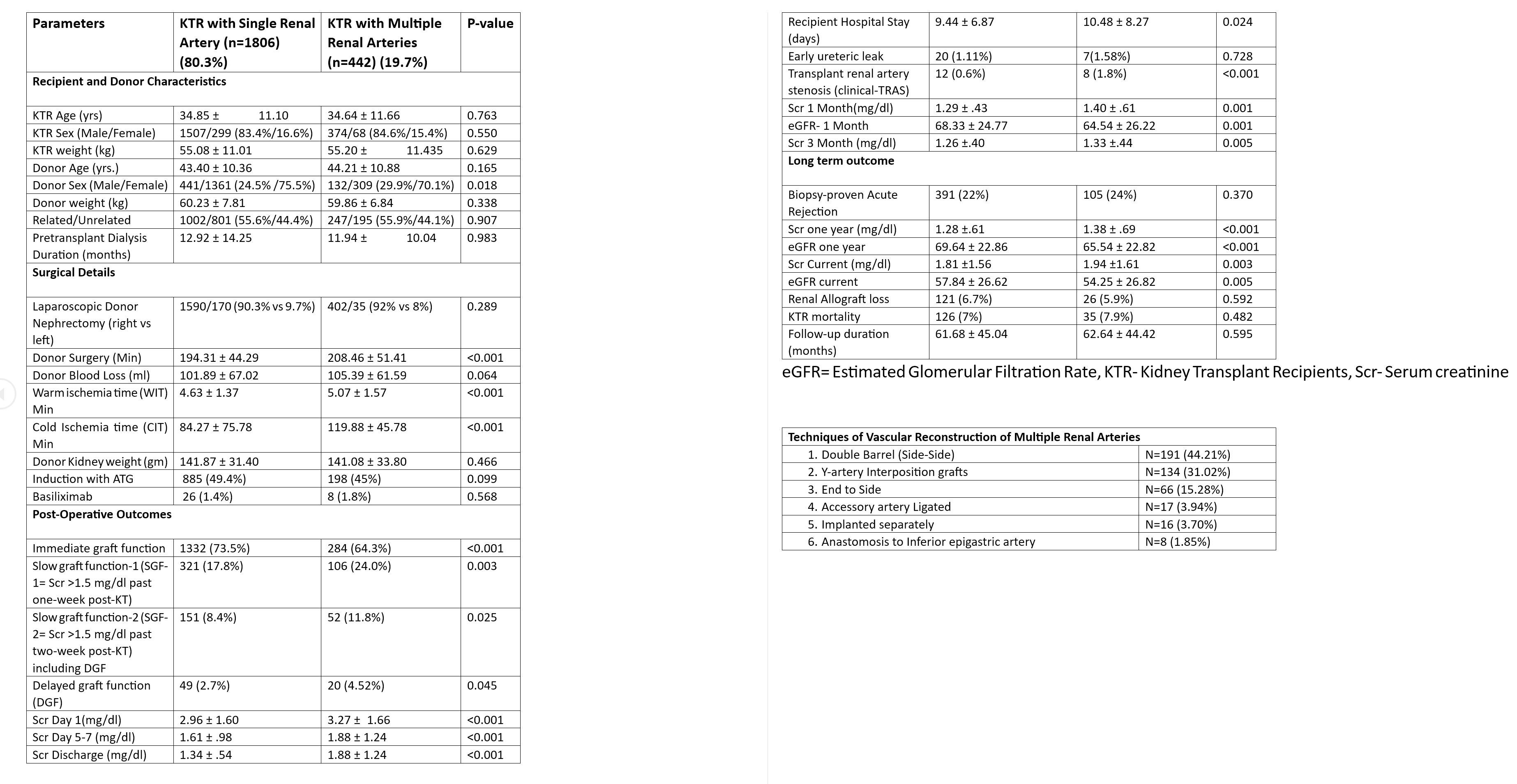
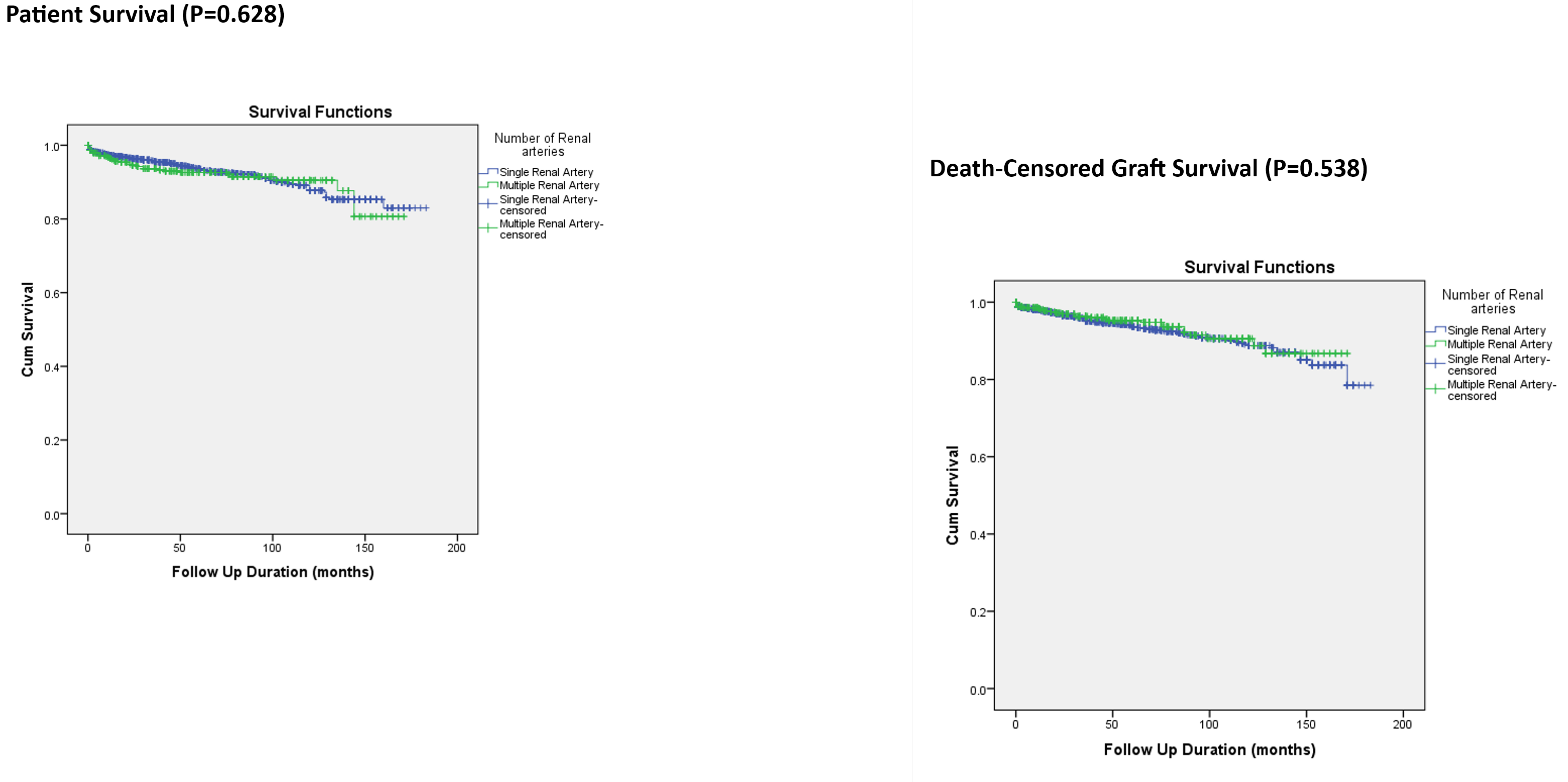
Results-Of the 2248 LDKT analyzed, 19.7% KTRs were transplanted with MRA-allograft, with 91.4% of the total MRAs underwent ex-vivo back-table vascular reconstruction. LD-KT recipients with MRA allografts experienced a statistically significant higher donor operating-time, warm-ischemia, cold-ischemia time, delayed graft-function(DGF), slow graft-function(SGF), and higher rates of vascular complications as transplant renal artery stenosis(TRAS) compared to KTRs with SRAs. Moreover, KTRs with MRA allografts had more extended hospital-stays and exhibited significantly higher mean serum creatinine(SCr) and lower mean estimated glomerular filtration rates(eGFR) at discharge, which continued across follow-ups at one-month, three-months, and from one to five years, relative to their SRA counterparts. However, there were no significant differences in early-urological complication, biopsy-proven acute rejection, death-censored graft-survival, and patient-survival over a mean follow-up of 61.86±44.91 months.
Conclusion-LDKT with MRA allografts compared to SRA allografts, although technically challenging and leads to elevated risks of DGF, SGF, and TRAS, did not negatively impact the long-term graft survival despite a slightly increased mean SCr and a decreased mean eGFR at discharge and during the one-year and five-year follow-ups.
[1] Living Donor Kidney Transplantation
[2] Laparoscopic living-donor nephrectomy
[3] Graft Survival
[4] Vascular Reconstruction
[5] Graft outcome
[6] Single Renal Artery
[7] Multiple Renal Arteries
