
Hospital admissions in the first 10-years of children born to transplanted mothers
Erandi Hewawasam1,2, Christopher Davies1,2, Zhuoyang Li4, Elizabeth Sullivan4, Stephen McDonald1,2,3, Shilpanjali Jesudason1,2,3.
1Australia and New Zealand Dialysis and Transplant Registry (ANZDATA), South Australian Health & Medical Research Institute (SAHMRI), Adelaide, Australia; 2Faculty of Health and Medical Sciences, University of Adelaide, Adelaide, Australia; 3Central Northern Adelaide Renal and Transplantation Services (CNARTS), Royal Adelaide Hospital, Adelaide, Australia; 4Faculty of Health and Medicine , University of Newcastle, Newcastle, Australia
Introduction: Despite rising births in kidney transplant recipients, their babies face elevated risks, including preterm birth and low birthweight, with over 50% being preterm and experiencing worse neonatal outcomes than other preterm babies, highlighting the importance of understanding its long-term implications beyond the neonatal period. We aimed to explore the long-term health trajectories of children born to transplanted mothers compared to those of mothers who had not received kidney replacement therapy (non-KRT).
Methods: We utilised linked data between the Australia and New Zealand Dialysis and Transplant Registry, perinatal (births ≥20 weeks gestation, 1991-2013) and hospital admission datasets (available until 2018) in four jurisdictions in Australia (South Australia, Western Australia, Australian Capital Territory and New South Wales).
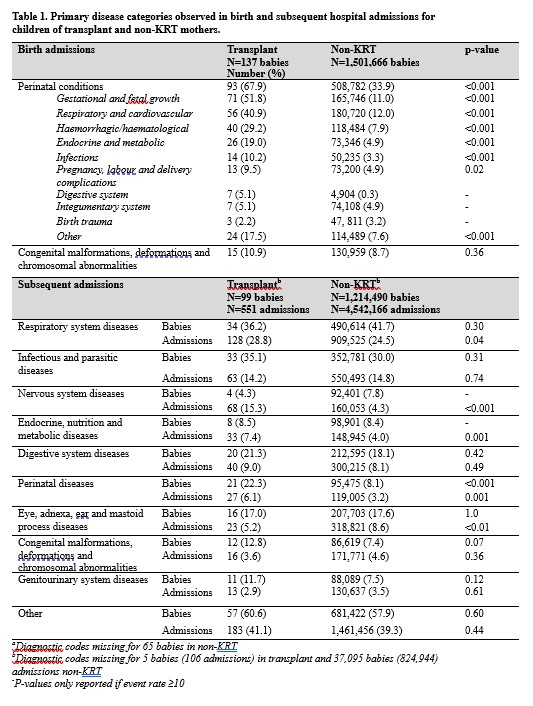
Results: Of 1,865,425 babies with 6,063,327 hospital admissions, there were 137 birth admissions and 551 subsequent admissions (n=99 babies) in the transplant cohort, with a median follow-up duration of 2.5 years [IQR: 0.9-5.3] compared to 2.9 years [1.1-5.4] in the non-KRT cohort (p=0.03). Neonatal deaths (<28 days post-delivery) were 3.5% in the transplant cohort (0.2% non-KRT), with just one post-neonatal death. Children of transplanted mothers experienced lengthier birth admissions (median 6 days [IQR: 4-16]) than those of non-KRT mothers (3 days [2-5]), p<0.001. Nearly 70% of children born to transplanted mothers (vs 34% non-KRT) had perinatal-related admissions, associated with gestational age/fetal growth issues, respiratory/cardiovascular diseases, haemorrhagic/haematological conditions, endocrine/metabolic disorders, infections and pregnancy complications, 2-5 times higher than the non-KRT cohort (p<0.05) (Table 1). Subsequent admissions for respiratory, nervous system, and endocrine/metabolic diseases were also more prevalent in children of transplanted mothers (7-29%) than the non-KRT (4-24%), p<0.05. Prematurity (57% Transplant vs 8% non-KRT) and pre-eclampsia (30% Transplant vs 6% non-KRT) were further explored as crucial factors affecting neonatal health. Preterm children of transplanted mothers showed heightened respiratory-related subsequent admissions (41%) compared to other preterm children (26%, p<0.001). Among women with pregnancy-induced hypertension (including pre-eclampsia), children of transplanted mothers had higher rates of perinatal conditions (80% vs 51%), endocrine/metabolic diseases (8% vs 4%), and respiratory diseases (35% vs 23%), p<0.05.
Conclusions: This first Australian follow-up study of children of transplanted mothers revealed prolonged hospital stays and a surge of perinatal-related conditions and respiratory diseases. These findings emphasise the need for ongoing monitoring to improve the long-term health of these children.
The Hospital Research Foundation Women’s Health Grant 2021. National Health and Medical Research Council, Australia, APP1173941. National Health and Medical Research Council, Australia, APP1092957.
[1] Pregnancy
[2] Kidney transplantation
[3] Hospitalization
[4] Follow-Up Studies
[5] Premature Birth
