Transplant outcome prediction by vascular lesions of deceased-donor kidneys
Junichiro Sageshima1, Karima Alghannam1, Naeem Goussous1, Neal Mineyev1, Ling-Xin Chen2, Richard Perez1, Kuang-Yu Jen3.
1Surgery, University of California Davis, Sacramento, CA, United States; 2Internal Medicine, University of California Davis, Sacramento, CA, United States; 3Pathology, University of California Davis, Sacramento, CA, United States
Introduction: Although the utility of donor clinical characteristics is well recognized, the additional value of kidney biopsy findings, especially vascular lesions, remains controversial in predicting transplant outcomes.
Methods: In this single-center retrospective study, permanent biopsy specimens taken at deceased-donor kidney transplants were scored by nephropathologists according to the Banff guidelines for arterial intimal fibrosis (cv), arteriolar hyalinosis (ah), hyaline arteriolar thickening (aah), interstitial fibrosis (ci), tubular atrophy (ct), and glomerulosclerosis (gs). First, we compared transplant outcomes based on the extent of donor vascular injury in the entire cohort and in a cohort matched on propensity score (PS) for donor characteristics. Next, we tested machine learning models (linear regression [LR] and light gradient boosting machine [LGBM]) to predict 1-year estimated GFR (eGFR) from donor characteristics alone or from biopsy findings in addition to donor characteristics.
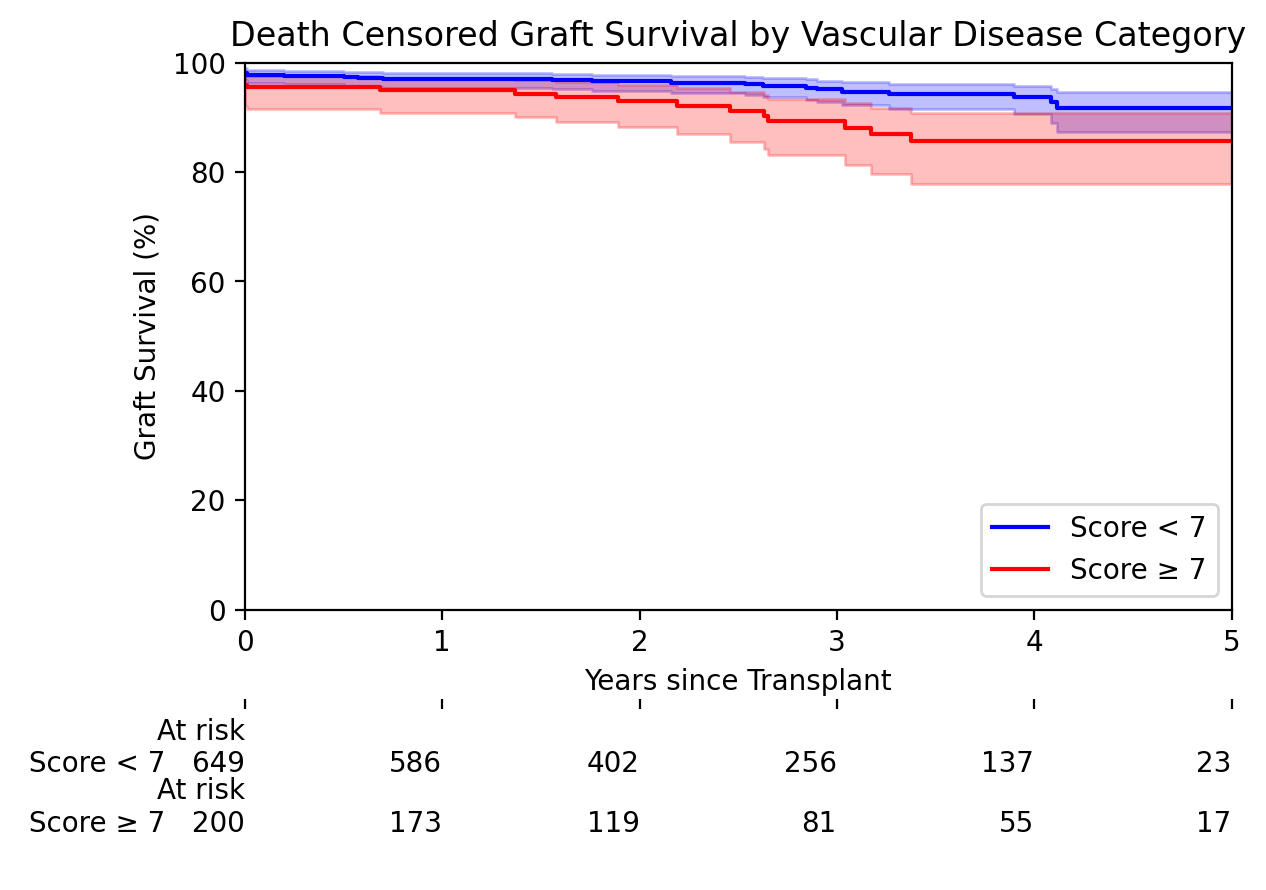
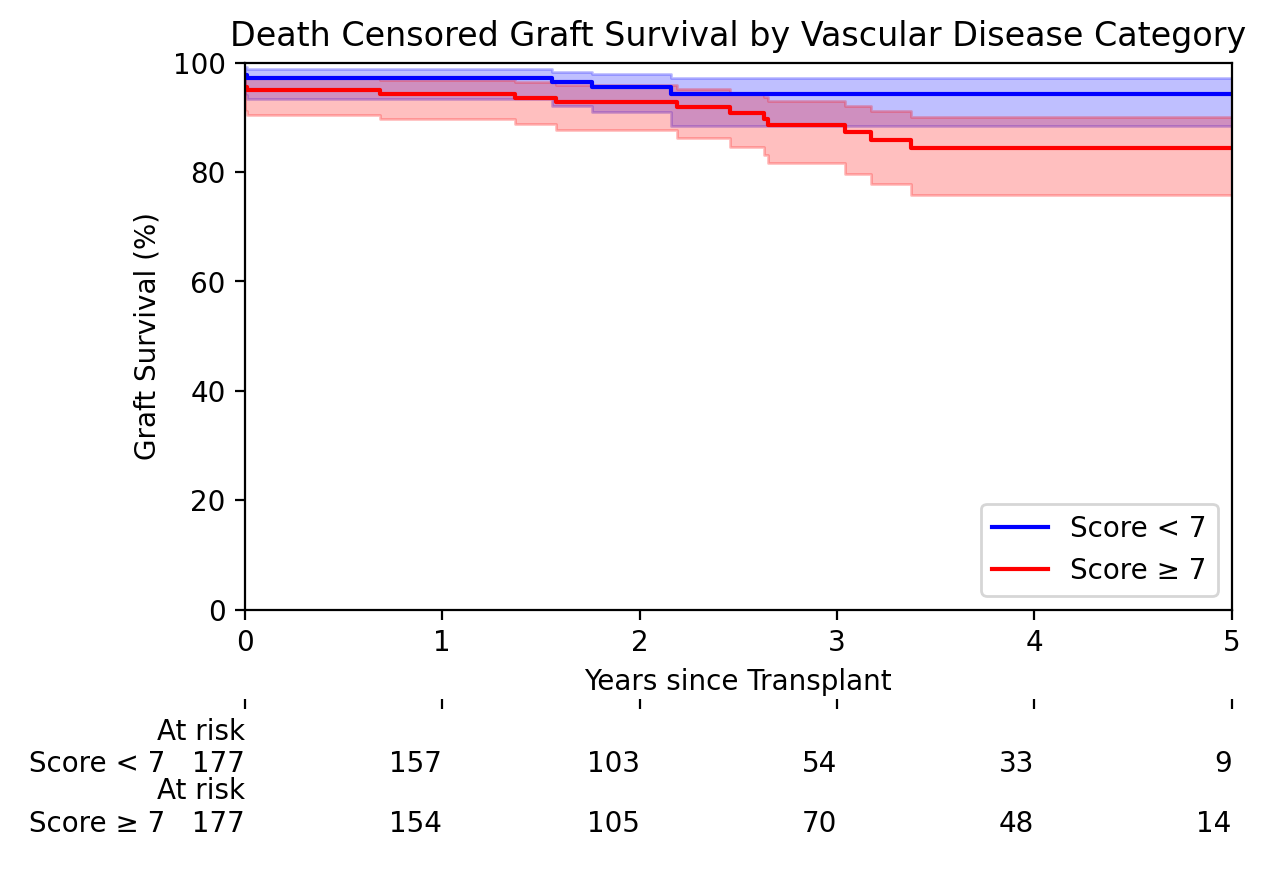
Results: During the study period (August 2017-July 2022), 851 implantation biopsies were available for analysis. When patients were categorized into two groups using the aggregated vascular score (2cv+ah+aah, ≥7 vs <7), 5-year death-censored graft survival was worse in the high score group: 86% vs 92%, p=0.01 for the entire cohort and 84% vs 94%, p=0.05 for the PS-matched cohort.
One-year eGFR was also lower in the high score group: 47±21 ml/min vs. 65±28 ml/min, p<0.0001 for the entire cohort and 47±21 ml/min vs. 54±23 ml/min, p=0.004 for the PS-matched cohort. Adding baseline kidney biopsy findings to donor clinical characteristics only slightly improved the eGFR prediction in both machine learning models – Root Mean Square Error: 24.1 vs 23.8 for LR and 19.0 vs 18.6 for LGBM.
Conclusion: When nephropathologists read baseline permanent biopsy specimens, deceased donor vascular lesions seem to be a valuable marker for predicting transplant outcomes at the population level; however, its utility in predicting kidney function in individual patients using conventional machine learning models may be limited.
