First experience of extracorporeal-cardiopulmonary resuscitation program and its impact in kidney transplant
Diana Colon1, Aroa Gomez-Brey1, Elisabeth Navas1, Maria Martinez3, Eduard Argudo3, Jordi Riera3, Irina Betsabe2, Francesc Moreso2, Bestard Oriol2, Alberto Sandiumenge1.
1Donation and Trasplantation Program Coordination Department, University Hospital Vall d'Hebron, Barcelona, Spain; 2Nephrology Department, University Hospital Vall d'Hebron, Barcelona, Spain; 3Critical Care Department, University Hospital Vall d'Hebron, Barcelona, Spain
Introduction: Extracorporeal-cardiopulmonary resuscitation (E-CPR) program is the final option for patients who do not respond to conventional cardiopulmonary resuscitation (CPR). In addition, it allows the possibility of fulfilling the will to donate in those patients who evolve unfavourably, thus increasing the pool of organs for transplantation
We present the analysis of viability and outcome of transplanted kidneys from deceased donors in the context of E-CPR.
Methods: Descriptive analysis of kidney recipients from all deceased donors at Vall d'Hebron University Hospital (HUVH) in 2023. Demographic data (donors and recipients), graft function and survival of all kidney recipients transplanted from E-CPR donors (E-CPR-D) was compared with that from brain death donors (DBD) and donors after circulatory death donors (DCD) due to other causes.
Results: Forty-nine E-CPR procedures were performed during the study period generating a total 15 actual donors (11 DBD, 1 cDCD, 1 donor after uncontrolled circulatory death donors [uDCD]) that accounted for a 20.5 % of all deceased donors (n=73). Two donors were not utilized and twenty-one kidneys and 6 livers were finally transplanted (2.1 valid organs per donor vs 2.9 DME vs 2.4 DAC).
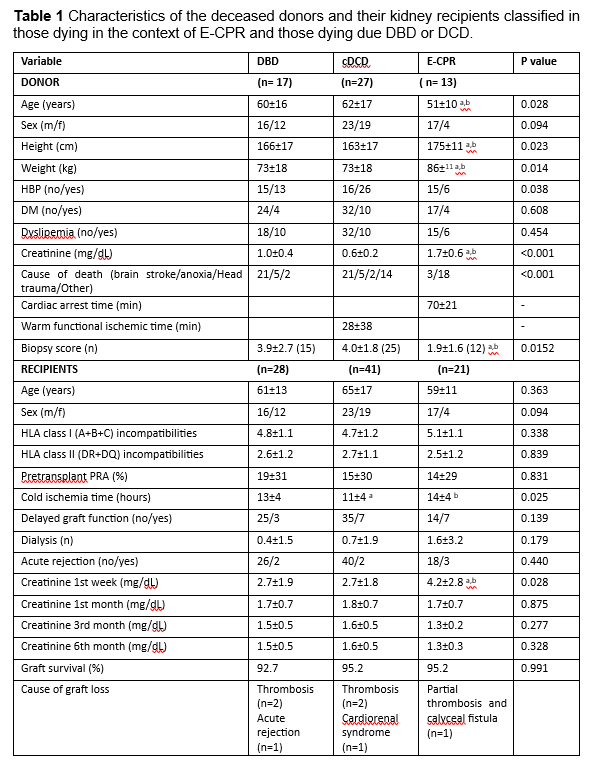
E-CPR-D were younger than DBD and cDCD. Although they had worse creatinine values at their initial assessment, kidneys obtained from E-CPR-D had better biopsy score compared to DBD and cDCD. (Table 1; donors).
Despite presenting longer cold ischemia times and higher creatinine values at first week, kidneys from E-CPR-D recovered function to values similar to those of DBD and cDCD with no differences in the % of delayed graft function (DGF) or acute rejection at 1-3-6 months follow-up (Table 1; recipients).
Conclusions: The E-CPR program at HUVH, in addition to offering a therapeutic opportunity to patients with refractory cardiac arrest, contributed to one out of every 5 real deceased donors in 2023. Kidneys transplanted from E-CPR-D showed similar functional results compared to those from donors of other types.
This paper was presented for consideration in the 8th National congress of the Sociedad Española de Trasplantes 2024 .
[1] ECMO-CPR
[2] Kidney recipient
[3] Organ donation
