The effect of normothermic machine perfusion and mesenchymal stem cells on porcine kidneys’ secretory profile
Maaham Saleem1, Kaithlyn M Rozenberg1, Marco Eijken3,6, Bente Jespersen2,3, Rutger J Ploeg1,4, Maria Letizia Lo Faro1, James Hunter1.
1Nuffield Department of Surgical Sciences, University of Oxford, Oxford, United Kingdom; 2Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 3Department of Renal Medicine, Aarhus University Hospital, Aarhus, Denmark; 4Department of Surgery – Organ Donation and Transplantation, University Medical Center Groningen, Groningen, Netherlands; 5Department of Urology, Aarhus University Hospital, Aarhus, Denmark; 6Department of Clinical Immunology, Aarhus University Hospital, Aarhus, Denmark; 7Department of Pathology, Aarhus University Hospital, Aarhus, Denmark; 8Department of Internal Medicine, Nephrology and Transplantation, Erasmus MC, University Medical Center, Rotterdam, Netherlands
Aim: Normothermic machine perfusion (NMP) is a novel organ preservation technique in transplantation. Alongside pumping the kidney with oxygenated blood at 37°C, NMP can also serve as a platform for the delivery of therapeutic agents such as mesenchymal stem cells (MSCs). In order to bypass issues associated with MSC administration in vivo, the delivery of paracrine factors secreted by MSCs in an ex-vivo setting is also an attractive therapeutic option. The MSC-derived secretome is not well characterised, particularly pertaining to which factors might be released during MSCs delivery by NMP. The focus of this study was to identify how concentrations of two well-known MSC-derived molecules (prostaglandin E-2, PGE2 and interleukin-10, IL-10) change during MSCs delivery to kidneys by NMP.
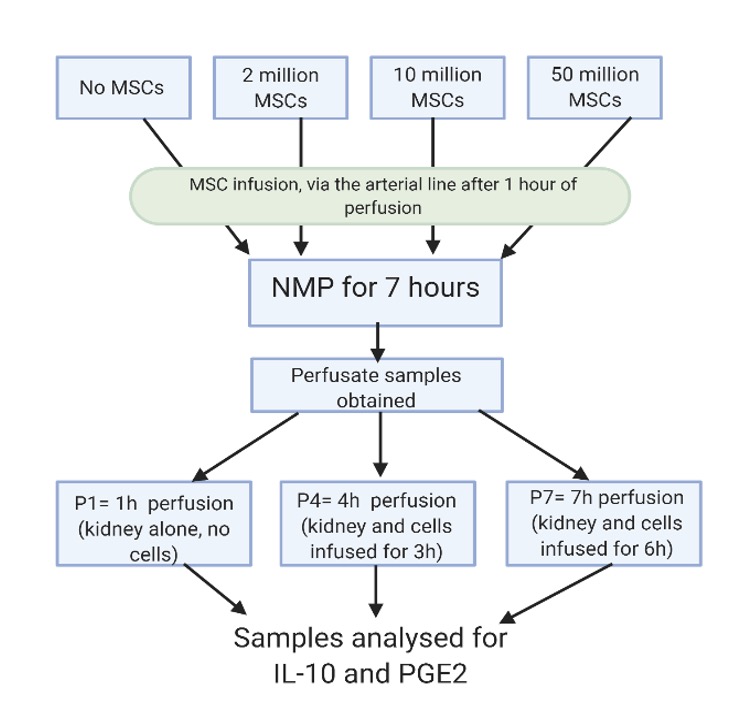
Materials and methods: A series of NMP perfusions were run with DCD-like kidneys being perfused for 7 hours and a differing number of MSCs (0, 2, 10 and 50 million cells) infused. Perfusate samples were collected at 1(P1),4(P4) and 7(P7) hours and analysed using commercially available ELISA tests for PGE2 and IL-10. The optical densities of standard PGE2 and IL-10 samples, of known concentration, were measured and used to plot a standard curve. Cytokine concentrations in the perfusate samples were interpolated from these curves. Statistical analysis was then performed using two-way ANOVA testing and Tukey’s multiple comparisons test.
Results: There was a significant increase in perfusate PGE2 concentration during NMP across all MSC dosages. Between P1 and P4, the most statistically significant increase in PGE2, observed in the group perfused with 10 million MSCs, was from 1.257 ±0.661 ng/ml (P1) to 16.85 ±2.34 ng/ml (P4) (p<0.0001). A rise in PGE2 with cell dosage was also observed at P4 and increased from 9.898 ± 0.764 ng/ml in the group with no MSCs to 16.85 ± 2.34 ng/ml (p=0.0454) in the 10 million MSCs group. No significant increase was observed between time points P4 and P7 (p>0.05), nor were any differences dependent on MSCs cell dosage observed other than at P4 as mentioned previously. Although a general increase in perfusate IL-10 concentration over time was observed, this increase was not found to be statistically significant (p=0.0681). No significant difference was found between IL-10 concentrations across MSC dosage groups (p=0.4465). At time point P7 the mean IL-10 concentrations in groups with 2 million and 50 million MSCs peaked, however they were not found to be significantly different from values measured at P1 (p=0.1679 and p=0.1459 respectively).
Conclusion: This pilot study indicates that a significant rise in perfusate PGE2 concentration occurs during NMP (and is increased by MSCs-infusion) while the role of IL-10 remains unclear, despite a potential trend towards increased levels in the presence of MSCs. Further studies are required to understand how NMP and cellular therapies can affect the kidney secretome and biology during preservation.
Members of the MEPEP consortium.
[1] NMP
[2] kidney
[3] mesenchymal stem cells
