Split Kidney Transplant from Pediatric donor < 18kg: Five years single center outcome analysis
Arun Panjathia1, Ashish Sharma1, Deepesh B Kanwar1, Sarabpreet Singh1, Shiv Kumar Patil1, Amit Sharma1.
1Renal and pancreas transplant department, post graduate institute of medical education and research, chandigarh, India
Introduction: Major concern in the treatment of end stage kidney disease patients is the organ shortage, although cadaveric transplant has provided a major relief to this growing problem. Using paediatric kidneys for adult renal patients has solved this major concern of shortage. Split paediatric kidney transplant has motivated the community to increase the transplant donor pool. Initially reluctance to use paediatric donor could explained by various factors, short term and long-term implications. High chances of urinary and vascular complications. Hyperfiltration injury and graft failure due to insufficient nephron number are the short-term implications. Anastomosis of vessels performed using aortic and Vana caval conduits and also exponential increase in the size of kidneys to increase in GFR. Splitting the paediatrics kidneys in order to expand the donor pool associated with technical risks also.
Material and methods: A single centre retrospective cohort study done from December 2017 to August 2022, Total number of transplants done were 922 and out of which deceased donor 233 during the study period. 14 split kidneys from 7 paediatric donors weighing less than 18 kg were transplanted into recipients. Patient data was retrieved from electronic database, telegram, case file and opd follow up in department of renal transplant surgery PGIMER.
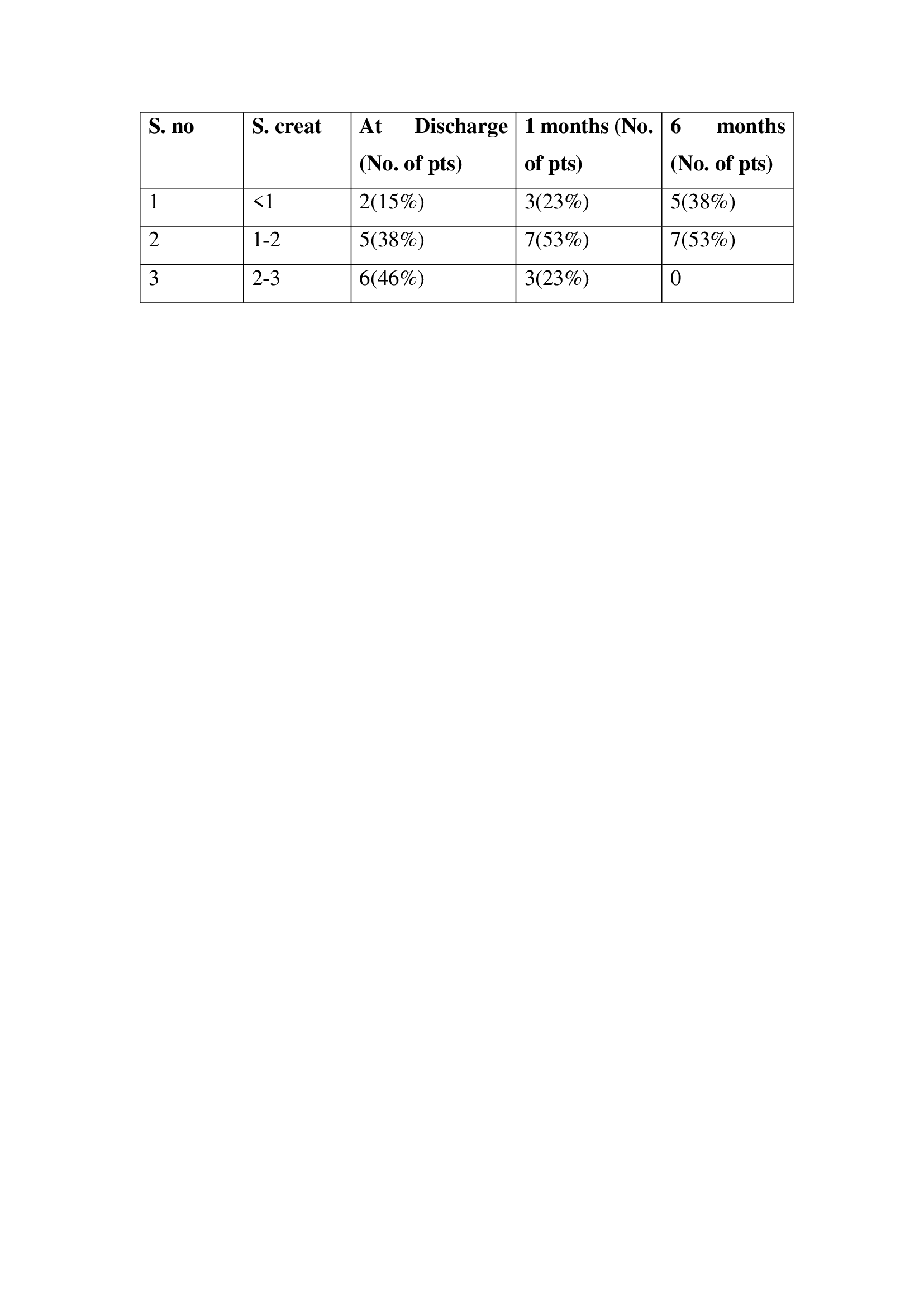
Results: The male and female recipients were (11:3). The mean (standard deviation [SD]) age of donors was 3.4 (1.1) years and recipients 27.7 (9.9) years. The mean (SD) estimated glomerular filtration rate increased steadily from 58 (31.8) mL/min/1.73m2 at the time of discharge to 116 (24.8) mL/min/1.73m2 at end of 12 months.
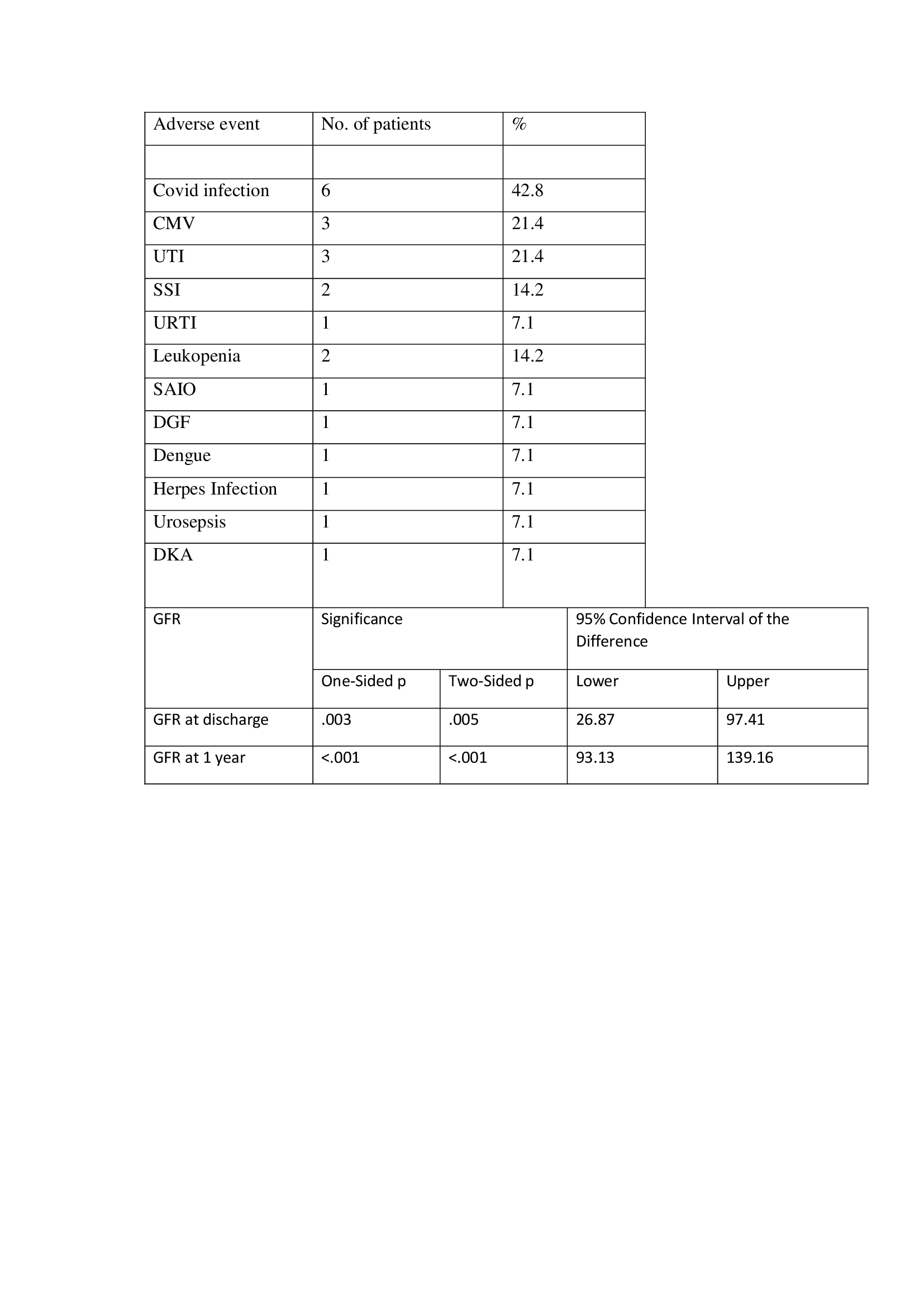
The mean (SD) eGFR remained stable at 24– and 36 months post-transplant with the decrease in mean (SD) eGFR to 104 (17) mL/min/1.73m2 at mean follows up of 31 (23.5) months. Rejection was noticed in 1/14 transplant recipients and 1/14 had Delayed graft function, no vascular and urinary complications were seen in any of the patients. 6/14 patients (42.8%) had covid infection post-transplant, 3/14 patients (21.4) had Urinary tract infection and 2/14 patients (14.2) had surgical site infection.
Conclusion: Split pediatric kidneys can contribute to the organ donor pool with good outcomes and robust graft function in long term but are associated with manageable adverse outcomes in short term and the technical difficulties can be dealt with good surgical skills of the operating transplant surgeon.
