Current status of ABO incompatible kidney transplantation in Japan: Based on statistical data of renal transplantation in Japan
Yuki Nakagawa1,2,3, Makiko Mieno2,3, Daiki Ogasa1, Naotsugu Ichimaru2, Hayato Hayato Nishida2, Michio Nakamura2, Kiyohiko Hotta2, Kazuya Omoto2, Masayuki Tasaki2, Taihei Ito2, Masayoshi Okumi2, Motoro Araki2, Takashi Kenmochi2,3, Shigeo Horie1.
1Department of Urology, Jntendo University Graduate School of Medicine, Tokyo, Japan; 2Registration Committee, Japanese Society for Clinical Kidney Transplantation, Tokyo, Japan; 3Registration Committee, The Japan Society for Transplantation, Tokyo, Japan
ABO incompatible kidney transplants have been performed since 1989 to expand renal transplantation in Japan, a country with a chronic organ shortage, accounting for 34.5% of all living donor renal transplants in Japan. Traditionally, it has been difficult to perform ABO incompatible kidney transplants in patients with high titers of anti-human blood group antibodies because of the high risk of antibody-related rejection.
In 1985, Alexandre et al. proposed plasma exchange (PEX) and dual filtration plasma exchange (DFPP) as a method to avoid antibody-associated rejection in ABO blood group incompatible renal transplantation. 6), immunosuppressive therapy with Rituximab plus PEX or DFPP for desensitization and antibody elimination without splenectomy has become the standard of care.
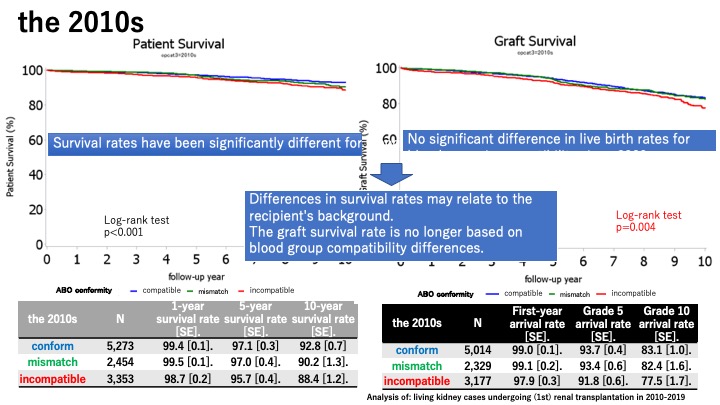
Results: In Japan, the 5-year and 10-year survival rates of ABO living donor renal transplantation since 2000 are 96.7% and 91.8%, respectively, and the 5-year and 10-year survival rates are 96.6% and 89.6% (death censored), respectively, which are comparable to blood group matched renal transplantation.
In 2021, 547 (35.6%) of living donor kidneys and 105 (87.5%) of donor kidneys were matched for ABO compatibility, and 310 (20.2%) of living donor kidneys were matched for incompatibility. Incompatible transplants were performed in 449 (29.2%) of the living kidneys. In a tally of special treatments for the 449 ABO-incompatible transplant cases of living kidney, splenectomy was performed in 2 cases (0.4%), plasma exchange in 366 cases (81.5%), immunoadsorption in 14 cases (3.1%), and immunoglobulin use in 55 cases (12.2%). The mean preoperative blood group antibody titers ranged from 16 to 32 times higher than that for blood group incompatible renal transplantation.
There was no significant difference in renal transplantation success rates according to preoperative blood group antibody titers.
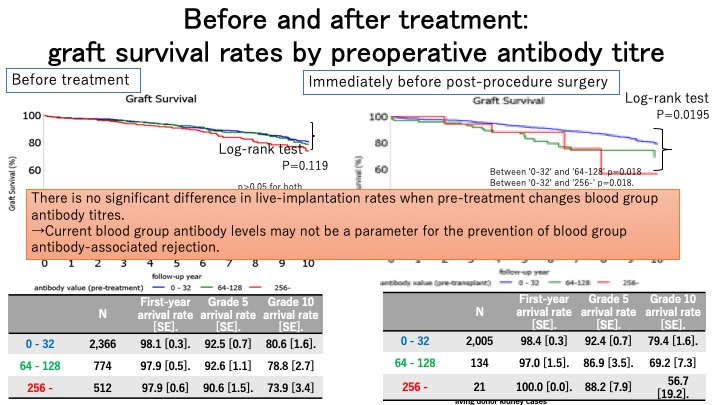
Conclusion: ABO incompatible kidney transplantation is increasing every year in Japan, where there is a chronic donor shortage. The proportion of PEKT is particularly high and often between married couples. There is no significant difference in blood group incompatibility between matched and matched recipients since 2000. There is no significant difference in the live-implantation rate between compatible and incompatible blood groups since 2000.
[1] The Japanese Renal Transplant Registry
[2] Renal Transplantations
[3] long-term dialysis patients
