Transplant renal artery stenosis: A potentially treatable cause of hypertension and renal allograft dysfunction
Kristine Gapuz1, Ruchi Naik1, Ignatius Tang1, Zahraa Hajjiri1, Walaa Dabbas1.
1University of Illinois Chicago, Chicago, IL, United States
Purpose: Transplant renal artery stenosis (TRAS) is a recognized vascular complication in kidney transplant recipients with an incidence of 1% to 23%. It occurs between 3 months and 2 years after kidney transplant, peaks in the first 6 months with a higher incidence in elderly patients. TRAS is considered as an important cause of allograft dysfunction and refractory hypertension following transplantation in 1-5% of patients. Donor artery atherosclerosis, suture techniques, traumatic or immunogenic vascular damage to donor or recipient arteries are identified as potential causes. Interventions by percutaneous transluminal angioplasty (PTA) with or without stent placement has a reported technical success rate of over 90% and clinical success rates ranged from 66% to 94%. We present a case series of 3 patients with TRAS occurred in different stages after transplantation with varying intervention and clinical outcome.
Methods: Retrospective review of electronic medical charts to identify cases of symptomatic TRAS. Baseline characteristics were collected, intervention and outcomes including blood pressure (BP) control and kidney function test following intervention.
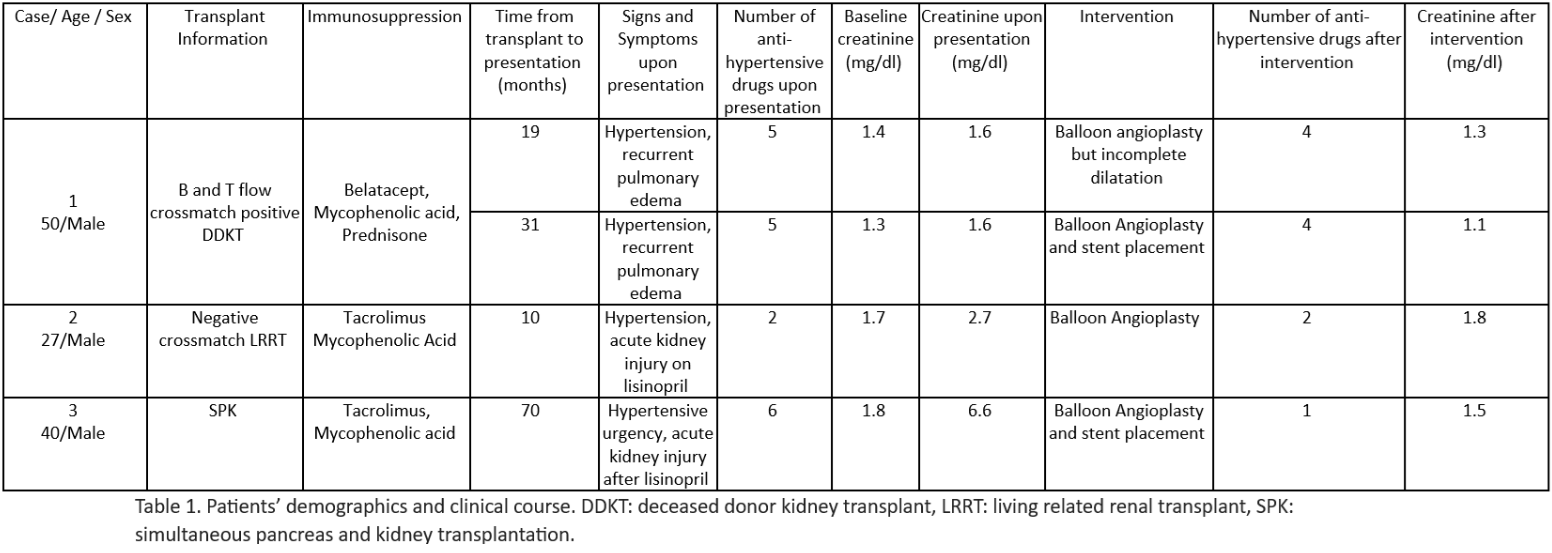
Results: Three cases were identified, all were male with an average age of 39 years at the time of diagnosis. One of the patients was post deceased donor kidney transplant (DDKT), one with living related renal transplant (LRRT), and the last one was a recipient of simultaneous pancreas and kidney transplant (SPK). Immunosuppression regimen included tacrolimus and mycophenolic acid except for 1 patient with biopsy proven tacrolimus toxicity, for which tacrolimus was replaced by belatacept. The time from transplantation to TRAS diagnosis was from 10-70 months. All patients presented with uncontrolled hypertension, pulmonary edema, and acute kidney injury (table 1). Patients 2 and 3, had acute kidney injury after starting Angiotensin Converting Enzyme Inhibitors (ACEi). Patient 1 has been on ACEi with recent increase in dose prior to TRAS diagnosis. Patients 1 had PTA with incomplete dilatation. There was minimal improvement in BP but kidney function and pulmonary edema improved. He presented 12 months later with recurrent pulmonary edema and hypertension. He underwent PTA with stent placement. He had minimal improvement in BP. However did not require further hospitalization for pulmonary edema. Patient 2 had trifurcation of main renal artery branches at the distal aspect of the narrowing that prohibited stenting due to risk of branch occlusion. He ended up getting PTA with balloon without stent placement. Patient’s 2 BP improved. Patient 3 had significant improvement in BP. All patients’ creatinine improved to their baseline.
Conclusions: TRAS can lead to graft loss, but early diagnosis and prompt intervention can lead to improved allograft survival and related systemic sequelae.