Advanced kaposi sarcoma with extensive pulmonary involvement after kidney transplantation
Walaa Dabbas1, Ahmad Nassar1, Ruchi Naik1, Mohammad Abuzeineh1, Paul Rubinstein1.
1University of Illinois Chicago, Chicago, IL, United States
Kidney transplant recipients (KTR) are at increased risk of cancer due to immunosuppression and impaired immunosurveillance. Kaposi sarcoma (KS) is a vascular tumor caused by human
herpesvirus 8 (HHV-8 / KSHV). The estimated incidence of KS in United states after solid organ transplantation (SOT) is 0.4% with a significantly higher incidence in KTR compared to other SOT recipients. Organ transplant-associated KS typically presents with cutaneous lesions. Visceral involvement as the initial manifestation of KS is an uncommon presentation. Pulmonary involvement is seen in AIDS-related but is rarely reported in SOT including KTR.
A 69-year-old African Caribbean 14 months post kidney transplant was admitted to a tertiary academic center for hemorrhagic shock following liver biopsy. The patient received a deceased donor kidney transplant with rATG induction and had been maintained on tacrolimus and prednisone. Mycophenolate mofetil was stopped early post-transplant due to foot osteomyelitis. Baseline creatinine between 2.1-2.5 mg/dl at 1 year post transplant.
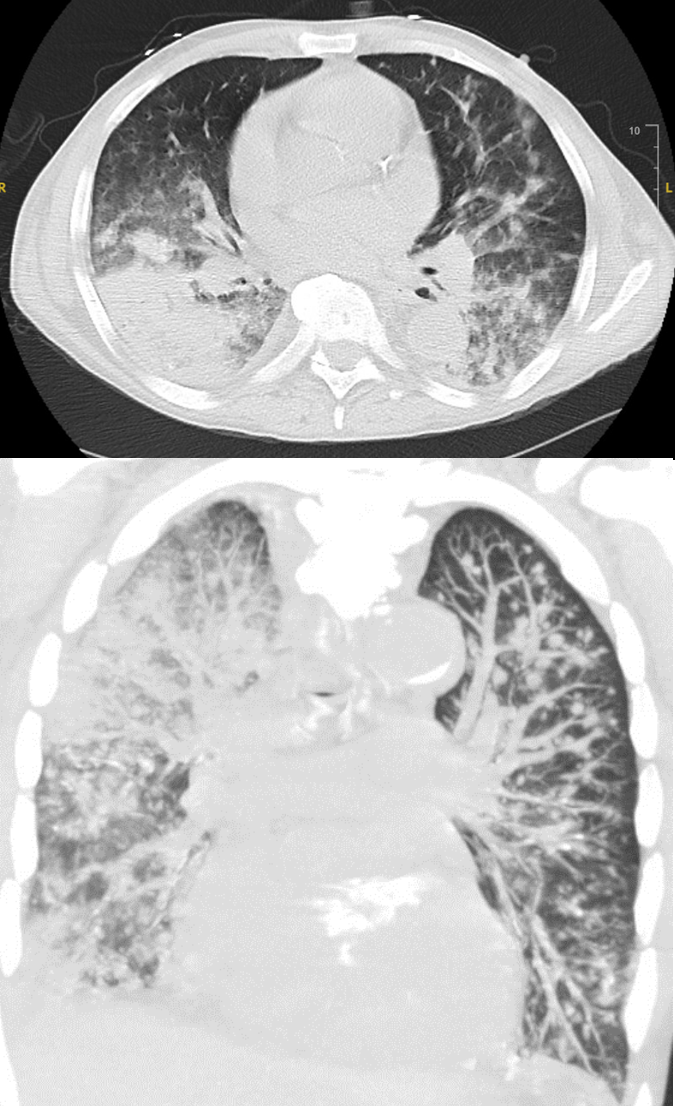
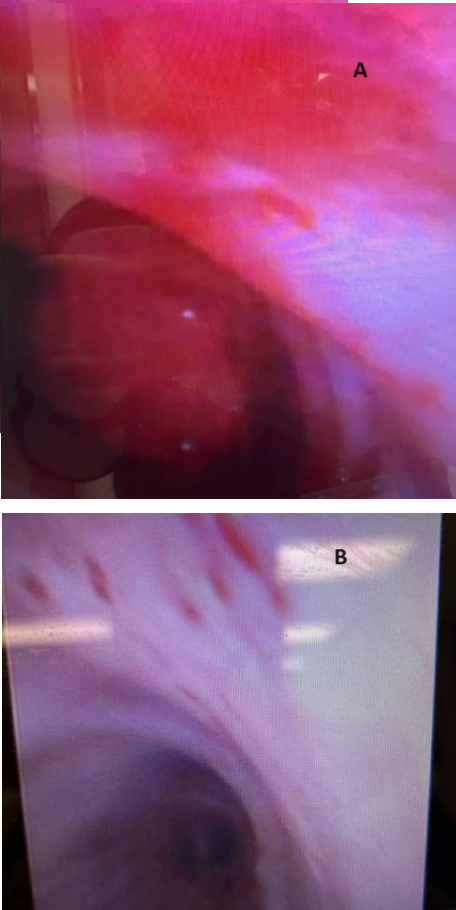
The patient underwent percutaneous liver biopsy for incidental numerous small ring enhancing lesions which was complicated by hemorrhagic shock requiring hospitalization and resuscitation with blood products and arterial embolization. One week later, patient developed acute respiratory failure. A chest computed tomography (CT) scan showed bilateral pulmonary opacities and diffuse bilateral small lung nodules. The patient’s respiratory status deteriorated despite broad-spectrum antibiotics. Bronchoscopy showed a mobile clot resulting in obstruction of the right mainstem and complete atelectasis of the right lung, the clot was removed. Postoperatively, patient had hemoptysis and respiratory failure requiring intubation. Repeat chest CT scan showed progressive pulmonary lesions and diffuse alveolar hemorrhage
Given immunosuppressed state, opportunistic infections were considered, serum HHV-8 was positive at 4400 copies/mL. Imaging of the body showed multiple enlarged lymph nodes (LN). An excisional biopsy of the right inguinal LN revealed a spindle cell neoplasm consistent with KS. Repeat bronchoscopy revealed multiple purple-red endobronchial lesions consistent with pulmonary KS. Diagnosis of advanced KS with pulmonary andLN involvement and probable liver involvement was made. Stage T1I0S1 according to the AIDS Clinical Trial Group staging system. Tacrolimus was switched to sirolimus and a dose of liposomal doxorubicin was given, however the patient’s clinical status worsened, and he expired.
Our patient had an unusual initial presentation of KS with pulmonary involvement. The patient’s extensive pulmonary disease at diagnosis and poor outcome related to the delay in diagnosis underline the importance of having a high index of suspicion for pulmonary KS in KTRs with unexplained respiratory manifestations. Early diagnosis and therapy are key in improving outcomes.