Heart transplantation following medically assisted dying using ex-vivo normothermic machine perfusion
Michael O'Leary1, Yashutosh Joshi2, Kelly Lewis3, Rodrigo Fritis-Lamora2, Claudio Soto2, Peter S Macdonald2.
1Organ and Tissue Donation Service, Sydney, Australia; 2Heart Transplant Unit, St Vincent's Hospital, Sydney, Australia; 3Organ and Tissue Donation Service, Concord Hospital, Sydney, Australia
Introduction: Patients with terminal illness electing for medically assisted dying (MAD) have the potential to donate organs following circulatory death. Successful heart procurement and transplantation after in-vivo cardiac reanimation using thoraco-abdominal normothermic regional perfusion (NRP) has been reported. NRP is associated with ethical concerns and may not be legal in some jurisdictions. We report the successful procurement and transplantation of a heart from a patient after MAD, with ex-vivo cardiac reanimation using normothermic machine perfusion (NMP).
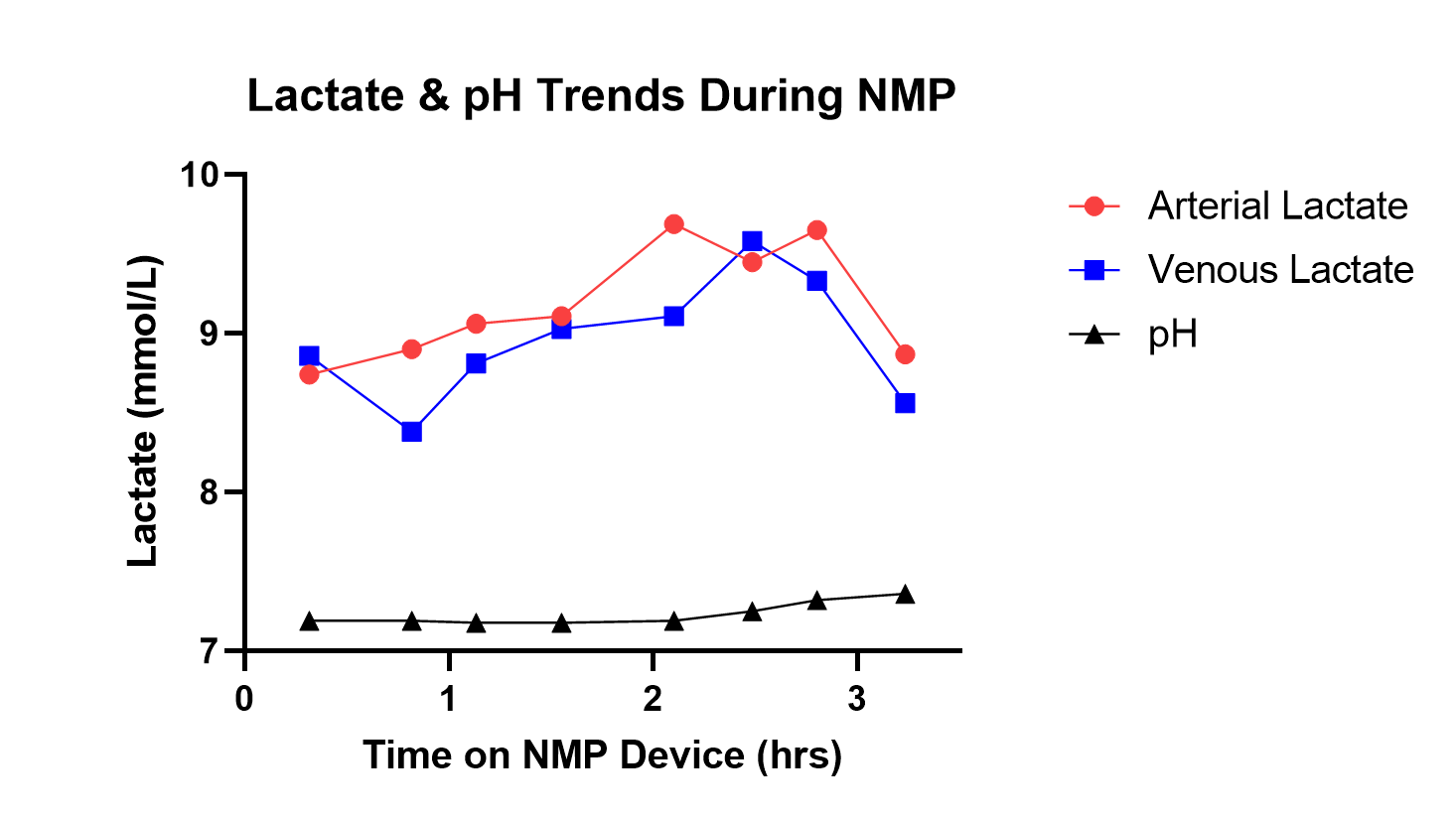
Methods: A 45-year-old male with a 2-year history of glioblastoma multiforme, WHO grade 4, and no other significant past medical history, was approved for MAD given short life expectancy and deteriorating functional status. He expressed a wish to donate his organs after death. He was admitted to hospital on his chosen date for MAD. In the anaesthetic bay of an operating theatre (OT) with his family in attendance, Heparin 55,000 units was administered two minutes prior to medications for MAD. Death was determined 5mins after electrical asystole on ECG, 19mins following administration of medications. The donor was transferred to the OT and the heart retrieved using a direct procurement protocol. Total asystolic warm ischaemic time prior to administration of cardioplegia was 10mins. Back-table cold ischaemic time was 32mins. The heart was perfused on the NMP device for 217mins. Donor heart viability was assessed using a combination of lactate profiles, NMP haemodynamic parameters and visual assessment of RV contractility.
Results: NMP perfusion following MAD was notable for point of care sampling demonstrating an upward lactate trend and associated metabolic acidosis up to 146mins. Given the presence of arterio-venous lactate extraction for the majority of NMP, satisfactory visual RV contractility, and haemodynamic performance, the decision was made to continue with the transplant. The heart was successfully transplanted into a 52-year-old male recipient following a re-do sternotomy and explant of a HeartMate3 LVAD. The recipient was weaned off bypass easily with no signs of acute primary graft dysfunction. ICU length of stay was 2 days. The patient did not require any form of dialysis and remained alive after >60days.
Conclusion: Successful heart transplantation after retrieval and reanimation using ex-vivo normothermic machine perfusion from patients undertaking MAD is feasible. Donor hearts following MAD may demonstrate atypical lactate profiles during NMP and although this did not seem to impair overall function, any potential pharmacotoxicity from MAD and its impact on NMP should be explored in future retrievals.
[1] Medically assisted dying
[2] Heart procurement
[3] Ex-vivo machine perfusion
[4] Heart transplantation
